If you’ve been diagnosed with liver cirrhosis, you may know that there are different stages of cirrhosis depending on how advanced your case is. If you’ve been diagnosed with stage 4 cirrhosis of the liver, you probably have many questions. What does it mean to have stage 4 liver cirrhosis, and what is stage 4 cirrhosis of the liver life expectancy?
Read on to find out the answers to your questions and what you need to know about stage 4 cirrhosis of the liver.
What Are the Stages of Liver Cirrhosis?
Let’s first look at the stages of liver cirrhosis to understand what it means to have stage 4 liver cirrhosis.
Stage 1 liver cirrhosis is the earliest stage of liver cirrhosis. While scar tissue is present in the liver, there is not enough damage to cause symptoms. Stage 1 cirrhosis of the liver is categorized as compensated cirrhosis. The healthy portions of the liver can function normally and compensate for the loss of function in damaged liver tissue.
Stage 2 liver cirrhosis is more progressed than stage 1. In stage 2, the portal vein in the liver stiffens, causing the blood pressure to go up. This condition is called portal hypertension. A damaged portal vein and blood vessels in the liver can cause blood to take different pathways through the body. For example, more blood may be rerouted through the blood vessels in the esophagus, causing esophageal varices.
Stage 3 liver cirrhosis marks the point at which cirrhosis now becomes decompensated, meaning that the liver can no longer function normally. At this stage, serious symptoms and complications of cirrhosis arise.
Stage 4 cirrhosis of the liver is the latest stage of liver cirrhosis. By stage 4, liver function is severely compromised, and the patient has reached end stage liver disease.
How Does Liver Cirrhosis Develop?
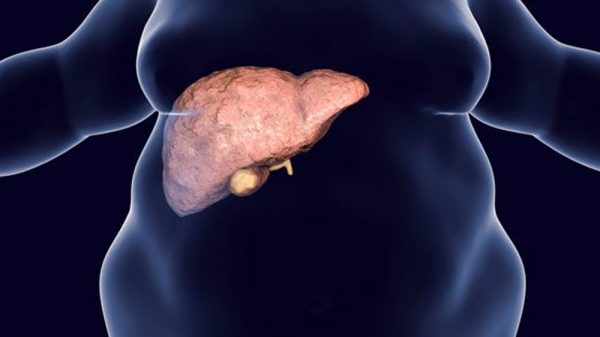
Liver cirrhosis develops due to a process called fibrosis. Liver fibrosis describes the production of collagen and scar tissue in the area surrounding liver cells. Over time, continued fibrosis causes healthy liver tissue to develop hardened areas due to scarred tissue. When the liver contains a buildup of scar tissue, this means that the liver has become cirrhotic.
It’s impossible for fibrosis and cirrhosis to develop spontaneously. Rather, scarring of the liver occurs as a result of chronic inflammation due to underlying chronic liver diseases.
- Chronic viral hepatitis: Viral hepatitis B or hepatitis C infection can cause inflammation in the liver that eventually leads to fibrosis and cirrhosis. Hepatitis B can usually be prevented by vaccination. However, chronic hepatitis C is more common.
- Alcohol abuse: Consuming large quantities of alcohol is one of the most common causes of liver cirrhosis in the United States. Alcohol is a toxin that the liver is responsible for metabolizing. Excess alcohol causes inflammation and oxidative stress in liver tissue. Over time, chronic alcohol abuse can cause alcoholic fatty liver disease, fibrosis, and cirrhosis.
- Nonalcoholic fatty liver disease: Nonalcoholic fatty liver disease is often associated with a sedentary lifestyle a diet high in sugar and saturated fat. Risk factors for developing nonalcoholic fatty liver disease include type 2 diabetes, insulin resistance, obesity, and other markers of metabolic syndrome. Fatty liver disease is characterized by fat accumulation in the liver that can eventually cause inflammation, fibrosis, and cirrhosis.
- Autoimmune hepatitis: Autoimmune hepatitis develops from immune system dysfunction. Normally, the immune system can distinguish between healthy tissues and infectious or harmful agents. However, when the immune system doesn’t work properly, the immune system may attack healthy organs. In autoimmune hepatitis specifically, the immune system attacks healthy liver tissue and over time causes inflammation, fibrosis, and cirrhosis.
- Hemochromatosis: Hemochromatosis is a genetic disorder that causes the body to absorb more iron than it needs. As a result, excess iron is deposited throughout the body, including the liver. Over time, iron deposits in the liver can result in inflammation and cirrhosis.
- Wilson’s disease: Wilson’s disease is a genetic condition that causes copper accumulation in different areas of the body, including the liver.
- Cardiac cirrhosis: Cardiac cirrhosis describes hepatic damage that develops due to cardiac issues, particularly heart failure.
- Biliary cirrhosis: Biliary cirrhosis, or biliary cholangitis, results from damage to the bile ducts. Bile ducts are responsible for carrying bile fluids from the liver to the gallbladder and small intestine. Damage in the biliary ducts causes bile fluids and toxic substances to accumulate in the liver, causing inflammation and cirrhosis.
Symptoms of Stage 4 Cirrhosis of the Liver
Symptoms of cirrhosis stage 4 are severe. Here are some of the symptoms and complications that you may be experiencing:
- Abdominal pain: Abdominal pain is a common side effect of liver cirrhosis. In particular, you may feel pain in the upper right quadrant of the abdomen, which is where the liver is located.
- Ascites: Ascites is the accumulation of fluid in the abdomen as a result of liver disease. Impaired blood flow through the portal vein also impacts the flow of fluids, causing excess fluid to become trapped in the peritoneal cavity.
- Hepatic encephalopathy: Hepatic encephalopathy is a condition that arises from the liver being unable to properly metabolize toxins. The liver is responsible for converting toxic ammonia into urea for excretion. However, when the liver can’t function properly, ammonia builds up in the bloodstream and travels to the brain, where it interferes with neurological functioning. Hepatic encephalopathy causes symptoms like confusion, anxiety, personality changes, impaired speech, abnormal movements, and seizures.
- Loss of appetite: Loss of appetite, nausea, and unintended weight loss are common side effects of advanced liver disease.
- Muscle wasting: The liver is responsible for many metabolic processes that help the body break down utilize nutrients from the food we eat. With the loss of liver function, the liver is no longer able to effectively process and distribute dietary protein. This causes the body to break down muscle tissue to gain access to essential amino acids for biological functions. Muscle wasting can cause weakness and fatigue and worsen the outcome of liver disease.
- Hepatorenal syndrome: Hepatorenal syndrome describes kidney damage that develops as a result of liver damage. Increased portal vein blood pressure and damage to surrounding blood vessels likely cause damage in renal blood vessels as well.
- Hepatocellular carcinoma: Hepatocellular carcinoma is a form of liver cancer. Individuals who have sustained significant liver damage like inflammation and scarring are at a higher risk of developing liver cancer. Early liver cancer stages are characterized by contained growths in the liver, while advanced liver cancer stages are characterized by metastasis to other organs.
- Esophageal varices: As described above, esophageal varices are bulging veins that develop from rerouted blood flow from the portal vein.
- Internal bleeding: You may experience internal bleeding like gastrointestinal bleeding with stage 4 liver cirrhosis. Increased pressure on the portal vein and surrounding vessels, as well as the reduced production of clotting factors, leave you at an increased risk for internal bleeding and easy bruising.
- Bacterial peritonitis: This bacterial infection affects the peritoneal cavity and develops as a complication of ascites.
- Jaundice: Jaundice is the yellowing of the skin that’s characteristic of advanced liver disease. When the liver no longer works properly, it is unable to break down bilirubin, which is a product of worn-out red blood cells. Bilirubin then accumulates in the body and causes a yellowish hue in the skin and whites of the eyes.
Stage 4 Cirrhosis of the Liver Life Expectancy
If you have stage 4 liver cirrhosis or liver failure, “how long to live?” is a common question. Stage 4 liver cirrhosis is a very advanced form of liver disease and is often life-threatening since liver function is severely compromised. However, the prognosis of your case of stage 4 liver cirrhosis is heavily dependent on the presence of complications and the extent of liver damage.
Physicians use the Child-Pugh scoring system of the model for end-stage liver disease (MELD) score to assess the extent of liver damage and to help determine a prognosis. The Child-Pugh score classifies liver disease based on bilirubin and albumin levels, blood clotting time, ascites, and hepatic encephalopathy. The MELD scoring system measures bilirubin levels, creatinine levels, sodium, and clotting time.
Your doctors will also likely order imaging tests to get a full picture of how your liver is working. Ultrasound technology, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans are important for evaluating the size of your liver and the presence of growths, scar tissue, inflammation, and other abnormalities. You may also undergo a liver biopsy, which requires removing a very small sample of liver tissue and using a microscope to analyze it for damage and abnormalities.
Blood tests will also be used to evaluate albumin, bilirubin, sodium, and liver enzyme levels.
If you are in liver failure and suffering from a broad range of severe complications, you may be told that you have months to live unless you can be given a new liver. On the other hand, if complications can be successfully managed, you may be told that you have a couple of years to live. In any case, it is critical to talk to your doctor to get the most accurate prognosis and survival rate for your condition.
Treating and Managing Stage 4 Cirrhosis of the Liver
Your treatment for stage 4 liver cirrhosis will be managed by a team of healthcare professionals. Your treatment team may include your general practitioner, hepatologist, gastroenterologist, nurses, and caregivers.
Treatment options include managing complications and minimizing further damage to the liver. To manage hepatic encephalopathy, you will be prescribed medications like rifaximin and lactulose to prevent gut bacteria from producing too much ammonia. You will also be prescribed diuretics to help get rid of excess fluid in the abdomen and legs.
You may also be advised to make diet and lifestyle changes that support liver health. For example, if your case of liver cirrhosis is a result of alcohol abuse, you will be advised to eliminate alcohol as part of your treatment plan. Eating anti-inflammatory foods can also help the liver sustain the function that it has left. For example, fruits, vegetables, whole grains, and healthy fats help reduce inflammation and oxidative stress throughout the body, including the liver. High-quality protein offers balanced ratios of essential amino acids, which can fight against harmful mechanisms in the liver and counteract muscle wasting.
It’s also crucial to follow all COVID-19 precautions since liver disease can make you more vulnerable to infection and the development of life-threatening symptoms.
Ultimately, liver transplantation will be part of your long-term recovery plan. A liver transplant entails removing your diseased liver and replacing it with healthy liver tissue from a donor. Undergoing a liver transplant requires a match with a living donor or an available liver from a deceased donor. Many individuals must wait for significant periods of time for a liver to become available.
Conclusion
Stage 4 cirrhosis of the liver is a severe and advanced form of liver disease. Stage 4 cirrhosis is often accompanied by debilitating symptoms like ascites, hepatic encephalopathy, and muscle wasting. A team of doctors and caregivers will help you manage your symptoms of liver cirrhosis, and you will likely need to undergo a liver transplant for the greatest chance of long-term success.