Shortly after you give birth to a child, the child is likely to develop physiologic Jaundice. It is quite common and is caused by a host of factors. The main factor, however, is that the child cannot yet excrete bilirubin properly from his or her body. As bilirubin builds up in your child’s body, the eyes and skin, as well as mucus would turn to yellow. The other common type of jaundice in newborn babies is pathological jaundice. Physiological (normal) jaundice usually resolves on its own and is not life-threatening. However, it is not so with pathological, jaundice which requires prompt medical treatment and could be life-threatening.
Physiological newborn jaundice may become serious or severe in rare occasions. But then, if it is properly monitored and managed, it should resolve by itself within 2 weeks. Complications from physiological newborn jaundice are usually more common in preterm or low birth-weight infants. The condition is often more severe in such newborns. But then, even full-term, normal birth-weight children have physiological newborn jaundice. As much as seven out of every 10 newborns in the U.S have this disorder. You could see that it is a very regular occurrence. What are the causes of this physiological disorder? How is it treated? What are the expected outcomes? These are the things we discuss in this article.
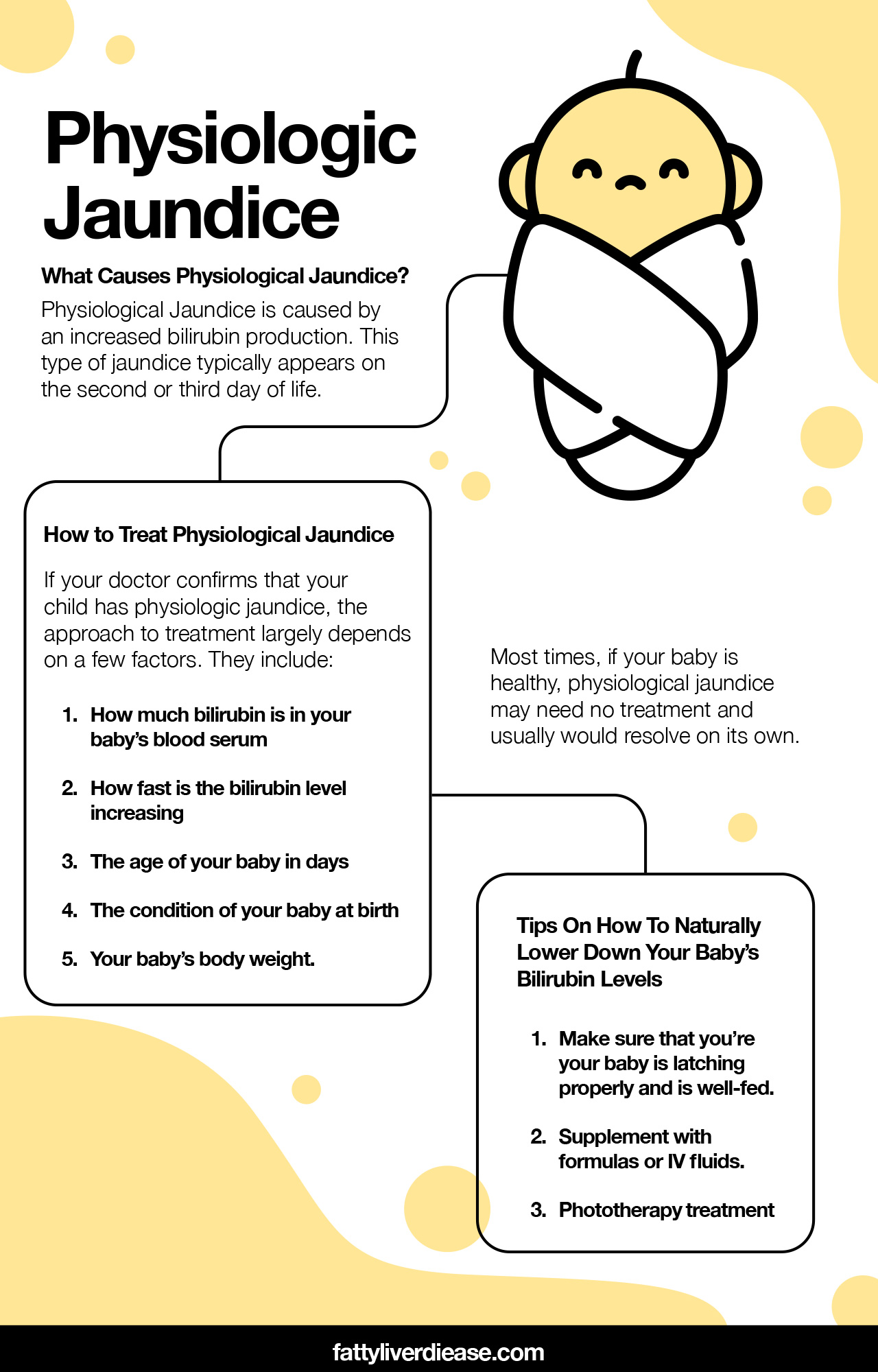
What Causes Physiological Jaundice?
To start with, newborn jaundice seems to have some genetic predispositions. It may run in families. So then, a baby whose siblings had physiological jaundice is more prone to having it.
Furthermore, a baby that is not feeding well also has an increased risk. This same holds when the mother is not producing enough milk. Even if these do not contribute to the disorder, they could make the condition worse.
Remember, however, that a risk factor is not the same as a cause. That your baby has more risk does not mean that he or she will have the condition. What a risk factor is that it increases the chances of having the condition.
Meanwhile, children that have no risk factor can still have the disorder. But then, if you notice any risk factor, you should talk about it with your doctor even before the condition shows up.
But then, what is the exact cause of physiological Jaundice? We will explain the entire process in a way that you can understand worn-out erythrocytes (Red blood cells or RBCs, for short) is a normal process. It occurs in the bodies of both adults and children.
When RBCs break down, it forms the waste product, bilirubin, which is a yellow pigment. On a normal day, your body excretes bilirubin after your liver processes it.
However, a newborn baby’s liver is not yet fully functional. It is immature and needs to develop a little bit more. As such, its efficiency in processing bilirubin for excretion is limited.
Because the liver cannot process bilirubin efficiently for excretion, there is left-over bilirubin in the baby’s body is not excreted. As bilirubin accumulates in the baby’s body, the yellow pigment begins to become more and more noticeable in the eyes, skin, and a few other parts of the baby’s body. This is how physiological jaundice develops.
As your baby feeds and the liver develops into maturity, it starts to function fully. And then, jaundice clears out naturally. This would happen within one to 2 weeks.
How to Treat Physiological Jaundice
Just as we mentioned earlier, physiological jaundice is usually not a serious disorder. It can clear up just be increasing breastfeeding.
However, you must not assume that jaundice in your baby is physiologic. You must allow the doctor to evaluate and assess your baby to be sure what form of jaundice your child has.
Firstly, your doctor would check the eyes, skin, palms, etc. of your bay under natural lighting conditions. If a yellow pigment is observed, then your child has jaundice.
Blood tests, urine tests, and urine culture are other means to evaluate jaundice. In the end, the doctor would be able to tell if your newborn’s jaundice is physiological or pathological.
If your doctor confirms that what your child has is physiologic jaundice, you can treat it as such. However, the approach to treatment largely depends on a few factors. They include:
- How much bilirubin is in your baby’s blood serum
- How fast is the bilirubin level increasing
- The age of your baby in days
- The condition of your baby at birth
- Your baby’s body weight.
That is why it takes an expert healthcare provider to examine and assess your baby. They are the ones who will tell you how exactly to treat the condition in your baby.
But then, most times, physiological jaundice may need no treatment of your baby is healthy. It usually would resolve on its own.
While your baby may not need any specific treatment, you may consider increasing the frequency of breastfeeding. This usually helps to bring down bilirubin levels.
You may have to learn proper techniques for latching and breastfeeding if need be. These would ensure that you’re your baby is sucking well and is well-fed.
If there are still issues with breastfeeding, you may supplement with formulas or IV fluids. But then, it is not up to you to decide. Your baby’s doctor would let you know if there is a need for any of these.
If bilirubin levels are becoming very high, the doctor may suggest phototherapy. This is a form of light treatment that helps to break down bilirubin in your baby’s body.
The doctor would expose your baby’s skin to a special kind of blue light. This light penetrates the skin, reacts with bilirubin, and breaks it down. That way, your baby will be able to excrete it.
Conclusion
Physiologic Jaundice is usually nothing to worry about. You can be so sure that the condition would improve and clear out as your baby begins to grow. All it takes is about one to 2 weeks for your baby’s liver to mature so that it can function to its full capacity.