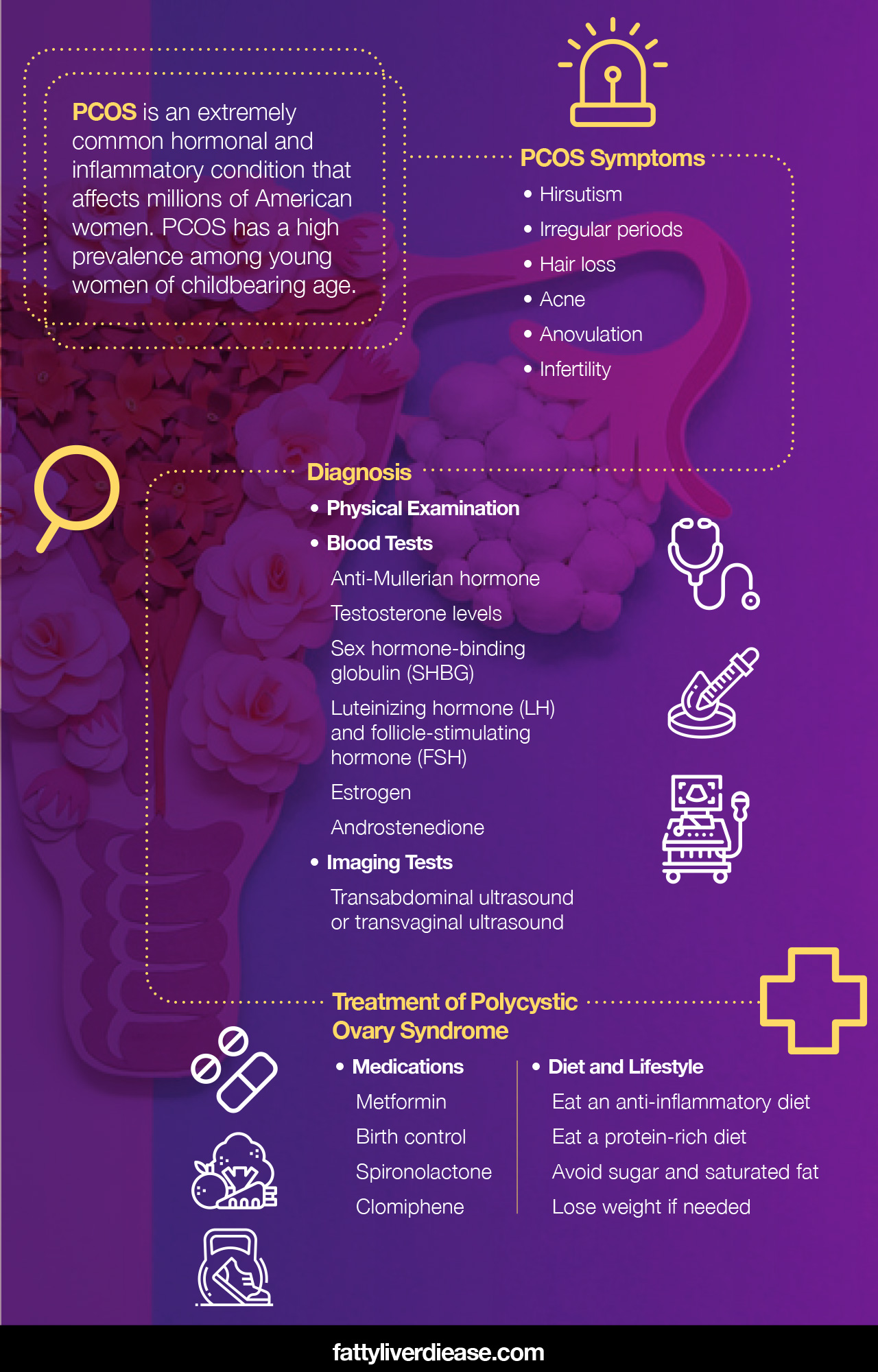
PCOS is an extremely common hormonal and inflammatory condition that affects millions of American women. PCOS has a high prevalence among young women of childbearing age. Although many articles on the internet discuss what you may experience with PCOS, there are few that discuss the diagnostic process and what to expect when you are evaluated for PCOS. If you want to learn about PCOS ultrasound findings, tests, and additional steps for PCOS diagnosis and treatment, then you’ve come to the right place.
Read on to find out more about PCOS ultrasound findings, blood tests, diagnostic criteria, and treatments for PCOS.
PCOS Summary
Let’s first quickly review what it means to have PCOS, also known as polycystic ovary syndrome or polycystic ovarian syndrome. PCOS is characterized by hormonal and metabolic dysfunction. Women with PCOS experience androgen excess and associated symptoms.
Symptoms indicative of PCOS include:
- Hirsutism: Hirsutism describes an abnormal pattern of hair growth. Male patterns of hair growth may affect women with PCOS, causing thick hair to grow on the face and chest.
- Irregular periods: Because hormones are not functioning properly, women with PCOS often experience irregular periods. This is because ovulation does not occur regularly, and the uterine lining does not thicken and shed each month. Some women with PCOS may have a period every few months, while others may experience amenorrhea (absence of a period).
- Hair loss: PCOS hair loss is a common symptom and results primarily from excess male hormone levels. Women with PCOS may experience hair loss and baldness.
- Acne: High androgen levels often cause breakouts in females along the jawline and lower cheeks.
- Anovulation: Hormonal imbalances often result in anovulation, which is the absence of ovulation during a menstrual cycle.
- Infertility: Because ovulation is irregular, infertility is a common symptom of PCOS. However, when PCOS is successfully treated, infertility can be reversed.
PCOS Diagnosis and What to Expect
Because PCOS is associated with numerous metabolic conditions as well as the endocrine and reproductive systems, the diagnostic process will likely evaluate many different aspects of your health. Let’s go through the strategies commonly used in the diagnosis of PCOS.
Assessing Symptoms
For many women with PCOS, inability to conceive, absence of a period, or bothersome hair growth and acne may prompt them to make an appointment with their gynecologist. Your physician will talk to you about your symptoms, and if you are experiencing any of the common symptoms, PCOS could be put on the table as a potential diagnosis.
Keep in mind that a woman may be experiencing an irregular cycle and infertility, without the signs of excess hair growth and acne.
Ruling Out Other Conditions
Your doctor will want a comprehensive understanding of your symptoms and will likely run several tests to ensure that you don’t have another condition. There are several other conditions that can cause symptoms that are similar to PCOS, including:
- Hyperprolactinemia: Hyperprolactinemia means that you have high levels of prolactin in the blood. High prolactin levels may cause
- Thyroid conditions: The thyroid is a small gland located in the neck and is responsible for regulating heart rate and metabolic rate. Thyroid abnormalities can cause high testosterone levels.
- Adrenal hyperplasia: Adrenal hyperplasia is a congenital condition that causes the adrenal glands to produce too many androgens, resulting in hyperandrogenism.
- Pregnancy: Pregnancy often causes changes in mood as well as a lack of a menstrual cycle. In some cases, these symptoms may be confused with PCOS. A physician may conduct a blood test for human chorionic gonadotropin (hCG), to make sure that pregnancy is not the cause of your symptoms.
Physical Examination
Your gynecologist may conduct a pelvic examination to check for abnormalities. A physical examination may reveal the presence of growths or enlargement of the ovaries. It can also help rule out other causes of symptoms and give the doctor a better picture of what’s going on.
Blood Tests
Blood tests are an important part of diagnosing PCOS. In particular, blood tests will look for the presence of excess testosterone in the bloodstream. There are several blood tests that can reveal hyperandrogenism or excess male hormones.
- Anti-Mullerian hormone: Anti-Mullerian hormone comes from ovarian follicles and is often elevated in women with PCOS.
- Testosterone levels: High testosterone levels are a key defining diagnostic finding in PCOS.
- Sex hormone-binding globulin (SHBG): SHBG binds testosterone, and women with PCOS tend to have lower levels of SHBG than normal.
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): Your physician may also order tests to evaluate other hormone levels in the body, to get a better sense of how your endocrine system is functioning. LH and FSH influence the menstrual cycle, ovarian follicle development, and the production of progesterone and estrogen. LH may be higher than normal in women with PCOS, while FSH may be lower than normal.
- Estrogen: Estrogen is a female sex hormone that may be higher than usual in individuals with PCOS.
- Androstenedione: Androstenedione is a hormone that is characterized as an androgen and may be found in elevated levels in women with PCOS.
Imaging Tests
A PCOS ultrasound is often conducted to reveal an image of the reproductive system and ovaries. Ultrasonography is a valuable technology that uses sound waves that bounce off tissues and create a sonographic image that the physician can use to search for abnormalities, especially in ovarian morphology.
Either a transabdominal ultrasound or transvaginal ultrasound may be used. In many cases, a transvaginal ultrasound may be performed, which can sometimes yield a better image of the ovaries. Images will be interpreted by a specialist in radiology.
The characteristics of a PCOS ultrasound of the female reproductive system include:
- Polycystic ovaries: Polycystic or multifollicular ovaries describe the abundance of excess follicles or cysts that develop on ovaries. It’s important to note that not all women with PCOS have polycystic ovaries.
- Follicle abnormalities: None of the follicles on the ultrasound are mature, and there is no dominant follicle, which is the follicle responsible for releasing an egg during ovulation. Instead, the number of follicles or follicle count is higher than normal.
- Enlarged ovaries: Women with PCOS tend to have ovaries that are larger than normal, which may also be referred to as having a higher ovarian volume.
- Thickened endometrial lining: Women with PCOS may have a thicker endometrial lining than normal, as shown by research. (1)
- Normal ovary ultrasound: It’s important to also keep in mind that a woman with PCOS may also have a normal ovary ultrasound. Not all women with PCOS have polycystic ovaries, enlarged ovaries, or extra follicles.
- Abnormal stroma findings: The stroma is an area of the ovary that is highly concentrated with blood vessels. Research shows that ultrasound findings in women with PCOS may have increased stromal blood flow velocity. (2)
Assessing for Associated Conditions
Many women with PCOS also experience comorbid metabolic conditions, like type 2 diabetes, insulin resistance, and fatty liver disease. Knowing the co-occurring conditions helps inform your physician for recommending the best and most comprehensive course of treatment, including medications, diet, and lifestyle changes. Here are a few markers of metabolic dysfunction that your physician may look for:
- High cholesterol and triglycerides
- High blood glucose
- High insulin levels
- Elevated liver enzymes
- Cardiovascular factors like high blood pressure
- Above-normal body mass index (BMI) or obesity
Rotterdam Criteria
Many physicians use the Rotterdam criteria in the diagnosis of polycystic ovary syndrome. The Rotterdam criteria include three diagnostic factors. Of the three factors, two must apply to the patient in order for PCOS to be a diagnosis. The three criteria are:
- Ovulatory abnormalities: Women with PCOS may have either irregular ovulation (oligo-ovulation) or a complete absence of ovulation (anovulation).
- Ultrasound findings: Polycystic ovaries may be a clinical finding in women with PCOS.
- Hyperandrogenism: Women with PCOS may present with high testosterone, which can be determined from biochemical tests or clinical presentation of symptoms.
Treatment of Polycystic Ovary Syndrome
If your physician has diagnosed you with PCOS, it’s now time to look at treatment options. Treatment usually entails a combination of both medication and diet changes. Specialists in endocrinology (endocrinologists) and gynecology and obstetrics (gynecologists and obstetricians) often treat PCOS. Here are a few recommendations and treatment options that your physician may suggest.
Medications
Medications can be extremely effective in managing PCOS. Here are a few medications that your physician may suggest:
- Metformin: Metformin for PCOS is used to help reduce insulin resistance, improve metabolic function, and improve blood sugar levels.
- Birth control: Birth control can be very helpful for regulating menstrual cycles in women with PCOS.
- Spironolactone: Spironolactone reduces excess testosterone and can help fight hirsutism.
- Clomiphene: Clomiphene is a treatment that is used to treat infertility in women with PCOS. Clomiphene encourages ovulation and increases the probability of conceiving.
Diet and Lifestyle
Diet and lifestyle changes are often encouraged for women with PCOS. Many women may even see a drastic improvement in symptoms with diet and lifestyle changes alone, without medications. Here are a few helpful diet alterations to consider:
- Eat an anti-inflammatory diet. Because PCOS is exacerbated by inflammation, eating lots of anti-inflammatory foods is a crucial aspect of the PCOS diet. Make sure your diet is filled with foods like fruits, veggies, whole grains, nuts, seeds, beans, lean meats, and fish.
- Eat a protein-rich diet. Protein helps slow down the release of sugar into the bloodstream, helping you avoid nasty blood sugar spikes and curbing insulin resistance. Protein also offers essential amino acids, which are needed to synthesize hormones, muscle tissue, and other biological compounds necessary for healthy metabolic and hormonal function.
- Avoid sugar and saturated fat. Cutting added sugars, refined grains, and saturated fat out of your diet can significantly improve metabolic function and inflammatory markers that worsen PCOS.
- Lose weight if needed. Weight loss is associated with improvement in hormone levels. You can encourage weight loss by eating an anti-inflammatory diet, eating the right number of calories for your needs, and incorporating more physical activity into your routine.
Conclusion: What You Should Know About PCOS Ultrasound, Diagnosis, and Treatment
A PCOS ultrasound is a valuable diagnostic tool. An ultrasound can reveal abnormalities on the ovaries in the reproductive system that are consistent with PCOS. In addition, blood tests can reveal hyperandrogenism and other hormone imbalances, as well as metabolic conditions associated with PCOS.
References:























