Opioid abuse is an epidemic in the United States. Opioids can be obtained medically, as doctors often prescribe them to treat pain following a serious surgery, injury, or chronic pain. However, opioid addiction can lead to taking too many prescription opioids and even obtaining substances like heroin and fentanyl illegally. Find out what it means to have an opioid overdose, including signs to look out for. You can also find out information about strategies for managing opioid addiction. Read on to find out more.
What to Know About the Opioid Crisis
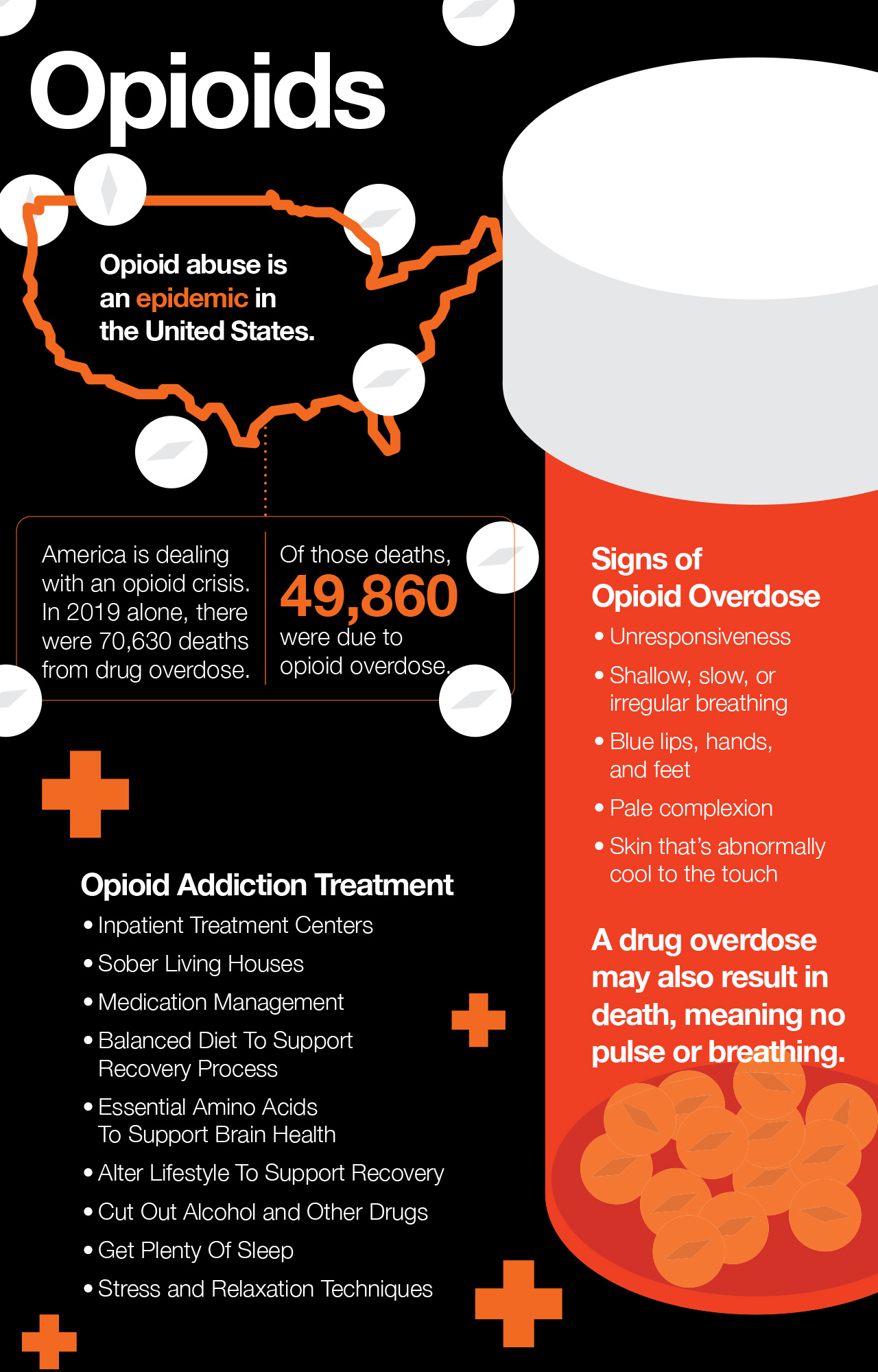
America is dealing with an opioid crisis. The Centers for Disease Control and Prevention (CDC) presents shocking health statistics and overdose data on opioid-related deaths. In 2019 alone, there were 70,630 deaths from drug overdose. (1) Of those deaths, 49,860 were due to opioid overdose. Opioid overdoses occur primarily as a result of synthetic opioids, both prescribed opioids and illicit drugs. (1)
What Does an Opioid Overdose Look Like?
Opioids are extremely dangerous substances because they can result in cardiac or respiratory arrest, which cause death. Opioid addicts are at risk of overdosing, especially when they are users of heroin or other opioid street drugs. Signs of overdose include:
- Unresponsiveness
- Shallow, slow, or irregular breathing
- Blue lips, hands, and feet
- Pale complexion
- Skin that’s abnormally cool to the touch
Keep in mind that a drug overdose may also result in death, meaning no pulse or breathing. In any case, time is of the essence and it’s important to call 911 for an overdose. When speaking to the operator, make sure you note that the victim is an opioid user and you suspect an overdose. First responders arriving on the scene will be able to administer naloxone – better known under the brand name Narcan – in order to reverse the overdose almost immediately.
The individual will still need to be taken to the emergency department, so that health care providers can monitor the person’s vital signs and overall health.
Similarly, if you have not heard from your addicted loved one for a period of time and you become worried, you should contact the authorities.
What Can Be Done to Support Opioid Overdose Prevention?
The U.S. Department of Health and Human Services (HHS) provides vital information for opioid overdose prevention. One of the primary recommendations is for family and friends of opioid users to carry Narcan, which can expedite the response time to an opioid overdose. (2)
The HHS also provides a link to a toolkit from the Substance Abuse and Mental Health Services Administration for health providers and loved ones of individuals struggling with opioid use disorder. One of the key recommendations for overdose prevention is treating the disorder itself. (3)
Let’s dive into strategies for treating opioid use disorder.
Can Opioid Addiction Be Treated?
Ideally, opioid addiction can be treated as a strategy for opioid overdose prevention. Despite the challenge of treating opioid use disorder and how relatively little is known about the disease, treatment options and healing strategies are available to treat the causes and effects of opioid abuse and addiction.
1. Inpatient Treatment Centers
Inpatient treatment centers are rehabilitation centers that are dedicated to helping individuals overcome addiction. When an addict enters a treatment center, the first step is to go through withdrawal. Stopping opioids cold turkey is an extremely difficult process both physically and emotionally.
Thankfully many clinics provide medically supervised withdrawal or partner with neighboring hospitals to accept patients who have undergone supervised withdrawal in a medical setting. After the physical dependence on opioids is broken, the underlying factors contributing to drug use can be addressed. Tending to underlying contributory factors in opioid addiction is the longest and most difficult part of recovery. This is why inpatient treatment centers are currently the most effective method for treating individuals suffering from substance abuse.
The typical stay in an inpatient treatment center is 3 months. In general, the longer patients remain in the treatment center, the better their chances are for remaining sober after leaving. While in a rehabilitation center, addicts receive intensive therapy to work through trauma and hardships that haven’t been dealt with. Working with a therapist and living in a rehabilitation center allows patients to learn and practice new coping skills, such as communication, journaling, artistic expression, and exercise. Many centers also help support healthy eating habits.
Inpatient treatment centers often offer psychiatric evaluations to detect any underlying mental health conditions like depression, anxiety, and mood disorders.
2. Sober Living Houses
Being surrounded by like-minded people with similar goals is tremendously helpful when navigating the journey to sobriety. A sober living house aims to provide a safe and sober environment for recovering addicts to live and reintegrate into society. Individuals living in sober houses might attend support groups together, work at local businesses, and enjoy hobbies together.
A large part of the success tied to sober living houses is the separation from familiar people and the comforts of home. Plus, sometimes the best thing for a recovering addict is to be separated from friends and family. Even if they have a wonderful and supportive family,
3. Medication Management
When transitioning out of rehabilitation and sober living, regularly seeing a psychiatrist who specializes in addiction and mental health disorders is critical to ensuring that underlying issues are managed appropriately.
For example, if an individual underwent a medical evaluation and was found to suffer from depression, visiting a psychiatrist regularly would ensure proper treatment with antidepressants and would allow the physician to keep tabs on any new or developing symptoms.
In some cases, a physician may decide that prescribing medication to curb your loved one’s desire to continue using opioids may be the best option. Suboxone and buprenorphine are popular drugs that operate like slow-release opioid medications that don’t deliver the “high” that opioid users experience. Suboxone, when used properly, can be effective in reducing drug cravings and balancing neurotransmitter activity that’s been disrupted by prolonged periods of opioid abuse.
Methadone is another opioid-based medication that is stronger than suboxone but produces similar effects. Suboxone, methadone, and buprenorphine interact with opioid receptors in the brain, which helps to make up for the shortage of natural opioids that exists after an individual abuses opioids for a prolonged period of time. Both Suboxone and methadone manage cravings without producing a euphoria or “high” that contributes to compulsive, unsafe use.
It would be ideal for an addict to rely on opioid-free methods of treatment, taking suboxone and methadone may be good stepping stones towards achieving that objective. keep in mind however that Suboxone and methadone can be abused. taking large amounts of these medications is a disservice to an opioid addict and sabotages their journey to sobriety. Suboxone and methadone should be administered by a doctor who believes that it will benefit the recovery journey. Addicts should never try to self-medicate with suboxone or methadone.
4. Nutrition
Nutrition is an important and often overlooked component of recovery from drug addiction. The foods we put into our bodies directly affect hormone balance and neurotransmitter balance. Eating a well-balanced diet supports healthy brain activity and helps the body heal from extended periods of drug abuse. Here are a few components of a diet that supports the recovery process from drug abuse.
Amino Acids
Amino acids are critical to supporting health and wellbeing. Nonessential amino acids can be found in food but aren’t nutritionally required because they can be produced endogenously by the body. Essential amino acids, on the other hand, must be consumed on a daily basis through the foods we eat. It’s well-known that amino acids are critical for numerous biological processes, including neurotransmitter synthesis, muscle growth, and enzyme production to carry out nearly all biochemical reactions. But did you know that amino acids can help directly in normalizing brain activity associated with addiction?
Dr. Charles Gant M.D., Ph.D., is a physician who specializes in addiction treatment and psychiatry. Dr. Gant has also researched the importance of nutrition in supporting a full recovery from opioid addiction. In his research, he has found that certain amino acids – including the essential amino acids leucine, methionine, and phenylalanine- play an important role in synthesizing neurotransmitters and endorphins that function as natural opioids. (4)
In particular, these amino acids serve as the raw materials used to produce healthy neurotransmitters and endorphins. Without the raw materials, the body is unable to synthesize the compounds needed for brain health, allowing the neurobiological effects of opioid abuse to persist.
So, where can you get plenty of essential amino acids to support brain health? A complete profile of essential amino acids can be found in all animal proteins, such as chicken, turkey, low-fat dairy, and fish. Essential amino acids can also be found in plant products, though only in incomplete ratios. As a result, a variety of plant-based proteins must be consumed throughout the day to ensure that you’re getting optimal ratios of essential amino acids to support neurotransmitter synthesis and brain health. A high-quality essential amino acid supplement can also help fill in any gaps in your diet.
Fruits and Vegetables
Fruits and vegetables are packed with healing compounds that support brain health when recovering from opioid abuse. Remember how opioid withdrawal results in unpleasant symptoms related to stress? Stress chemicals are released during withdrawal. The foods you eat can help you manage the stress symptoms and help your brain regain balance as you progress through the stages of recovery.
Stress symptoms associated with opioid withdrawal also cause physiological effects on the body. These effects are the direct result of a condition called oxidative stress. Excess epinephrine can cause your cells to go into overdrive. as your cells work hard in response to the presence of stress hormones, they generate more waste products such as reactive free radicals. These free radicals interact with healthy cells, including brain cells. Oxidative stress in the brain can exacerbate the symptoms of opioid withdrawal and can also slow down the process of healing from opioid abuse.
So, how can you mitigate the effects of oxidative stress? Though there are many ways to handle oxidative stress, changing your diet is one of the most effective methods. Fruits and vegetables in particular are filled with antioxidants that disarm free radicals and help the body get rid of them. Eating plenty of fruits and vegetables on a daily basis during recovery will help mitigate oxidative stress in the brain and help promote relaxation, lower levels of anxiety, and neurological repair.
What kind of fruits and vegetables should you be eating? Any and all kinds. Getting several servings of fruits and veggies from each color group each day will ensure that you’re getting tons of polyphenols, carotenoids, vitamins, and minerals that are needed for neurological repair. Reach for fruits and veggies like apples, beets, peppers, grapes, sweet potatoes, papaya, pineapple, mango, banana, avocado, kale, spinach, broccoli, and cauliflower.
Omega-3 Fatty Acids
Omega-3 fatty acids are polyunsaturated fats that are critical for supporting brain health. There are three types of omega-3 fatty acids: eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). The brain requires omega-3 fatty acids to fortify cell membranes and support nerve cells and neurotransmitters.
On top of that, omega-3 fatty acids are critical in lowering systemic inflammation. In turn, consuming plenty of omega-3s may help a recovering addict rebuild healthy neurotransmitters and signaling pathways.
So, where can you get plenty of omega-3 fatty acids in your diet? There are a few primary sources of the omega-3 fatty acids. DHA and EPA are derived from fatty fish like mackerel, salmon, Arctic char, cod, and anchovies. ALA found in plant-based foods like flaxseeds, chia seeds, walnuts, and pecans.
5. Altering Lifestyle
Making lifestyle changes that support recovery is critical to supporting recovery from opioid addiction. Here are a few strategies you can employ to support a sober lifestyle.
Exercise
Regular, vigorous exercise can help an individual recover from opioid addiction. Exercising has natural anxiety-reducing effects. Plus, exercising also encourages the brain to produce endorphins, also known as natural opioids.
Moreover, regular exercise is important for promoting physical health. Regular exercise is associated with improved cardiovascular health, a lower incidence of obesity, and better insulin sensitivity and liver health.
Cutting Out Alcohol and Other Drugs
When recovering from opioid addiction, it could be tempting to replace one sedative with another. Alcohol and other medications like benzodiazepine operate in a similar way to opioids by reducing anxiety. However, drinking alcohol and using other drugs can worsen the brain imbalances that accompany opioid abuse. Drinking interferes with normal neurological activity and strips the brain of omega-3 fatty acids and other essential nutrients that are necessary for repair.
On top of that, alcohol consumption also has inflammatory effects on the liver, heart and brain. A healthy recovery from opioid addiction should really be free of all substances, including alcohol.
Sleeping Regularly
Getting plenty of sleep is vital for supporting recovery from opioid addiction. While we sleep, the body is hard at work repairing damaged tissues. Plus, getting plenty of sleep helps us manage stress and recover from the day’s activities while preparing us for the following day. Maintaining a regular sleep schedule is also associated with better mental health.
Stress and Relaxation Techniques
Stress and relaxation techniques comprise a vital part of the recovery process from substance use disorder. Ongoing opioid abuse can result in disruptions in normal neurotransmitter activity, as discussed above. As a result, anxiety and emotional processing mechanisms won’t be working as well as they should. feelings of anxiety and being overwhelmed can increase the chances of experiencing cravings and increase the likelihood of relapse.
What kind of stress and relaxation techniques can be used as coping mechanisms? A few ideas are listed below.
- Yoga: In Eastern medicine, yoga has been used as a therapeutic practice for centuries to heal both the mind and soul. Practicing yoga helps center your thoughts and bring your consciousness back to the present moment. Stretching and maneuvering your body can also help the mind relax since it must focus on body movements. Your yoga practice can be tailored to your physical and mental needs.
- Meditation: meditation is a therapeutic practice for anyone struggling with emotional trauma, underlying mental health issues, anxiety, and substance abuse. Meditation is a calm state that allows your mind to freely exist in the present moment, and simply “be.”
- Deep breathing: Deep breathing can be used during meditation or on its own. Deep breathing has profound effects on the physiological effects of anxiety. For example, taking slow, deep breaths calms your heart rate and helps lower your blood pressure.
Conclusion: What Does It Mean to Have an Opioid Overdose?
The opioid epidemic is a public health crisis in the United States. Opioid overdose is life-threatening and requires immediate medical attention and the administration of Narcan. First responders carry Narcan to prevent opioid overdose deaths. Family members and friends of opioid users can carry the life-saving medication and shorten response times even further. Treatment and interventions for opioid use disorder is the most effective strategy for preventing drug overdose deaths.
References:
(1) https://www.cdc.gov/drugoverdose/deaths/index.html
(3) https://store.samhsa.gov/sites/default/files/d7/priv/sma18-4742.pdf