Being diagnosed with fatty liver disease is unsettling. Does such a diagnosis mean you are inevitably bound for liver failure, or can liver damage be reversed? What is NASH liver disease life expectancy? Luckily, fatty liver disease and liver damage are reversible. Here we go over everything you need to know about the course of fatty liver disease.
What You Should Know About Fatty Liver Disease at the Time of Diagnosis
If you have just been diagnosed with fatty liver disease, don’t panic. During these early stages, you are not facing an impending health crisis. Fatty liver means that fat particles have accumulated in your liver, and as an isolated condition, the fatty liver does not pose an immediate health risk.
At this point, medical interventions that directly target the liver are typically only available for very advanced cases of liver disease.
Even though there are virtually no medical options for treating fatty liver in the early stages of fatty liver disease- and even in later stages – there are numerous diet and lifestyle changes that can support liver health, regeneration, and reversal of the disease. It’s important to make these changes to prevent fatty liver disease from progressing to more serious, life-threatening diseases.
Let’s take a look at the different stages of nonalcoholic fatty liver disease.

Early Stages: Nonalcoholic Hepatic Steatosis
Hepatic steatosis is the scientific term that describes the buildup of fat in the liver. Nonalcoholic fatty liver disease (NAFLD) and nonalcoholic hepatic steatosis are synonymous terms for describing the same condition. NAFLD is an extremely common condition around the globe, and in North America, fatty liver disease is estimated to affect up to a third of the population. (1) At the early stages, there are usually no symptoms.
Nonalcoholic Steatohepatitis
After years of fat accumulation in the liver, it is possible to develop nonalcoholic steatohepatitis (NASH). NASH describes the condition that occurs when fat accumulation over time leads to liver inflammation.
Inflammation describes an overactive immune response that can lead to tissue damage. Fat accumulation in the liver can aggravate liver cells and trigger immune mediators like cytokines, which then become chronically activated and impede normal cellular processes. Oxidative stress is another factor that contributes to inflammation. When your liver is constantly processing an overload of fats, sugars, chemicals, and other compounds, damaging particles called free radicals build up within cells. These free radicals are reactive and inflict damage on biological structures.
Liver Fibrosis and Cirrhosis
Years of chronic inflammation and liver damage leads to the development of scar tissue. Fibrosis is the term that describes the accumulation of collagen and other tough cellular materials that form scars. Over time, fibrosis may cause so much scarring that it results in cirrhosis. While a normal liver is soft and spongy in texture, a cirrhotic liver contains hard, fibrous scar tissue that impairs liver function.
Liver Cancer
In some cases, chronic liver damage not only leads to the loss of function but also the growth of malignant cells. Liver cancer, or hepatocellular carcinoma, may develop as a result of liver cirrhosis. Cancerous growth in general results from the replication of faulty DNA. A short background on cancer biology helps explain why liver cirrhosis increases the risk of liver cancer.
Every cell throughout the body contains DNA – your unique genetic code that contains instructions for producing proteins that are responsible for carrying out all biological functions and define your characteristics. Naturally, cells get old and worn out and must be replaced. When cells divide to replace old cells, your body must produce perfect copies of the DNA. Mistakes happen, and sometimes pieces of replicated DNA contain deletions, substitutions, and other errors. Normally, there are many protective and corrective mechanisms built into our bodies that correct “broken” DNA strands or induce cell death – “apoptosis”- to prevent the growth of damaged cells.
In the case of cancer, however, these cells with faulty DNA begin to proliferate. Chronic injury to a certain organ makes it more likely that the normal protective mechanisms for preventing cancer are not working properly. Liver cirrhosis is, therefore, a significant risk factor for developing liver cancer. Liver cancer causes the mass accumulation of malignant cells and the creation of tumors, which further inhibit normal function. Liver cancer can ultimately lead to end-stage liver disease and liver failure.
End-Stage Liver Disease
When liver damage or cancer progresses to the point of nearly complete loss of function, this is called end-stage liver disease. Serious symptoms and complications are associated with end-stage liver disease. For example: swelling in extremities, ascites, hepatic encephalopathy, kidney failure, jaundice, and bruising.
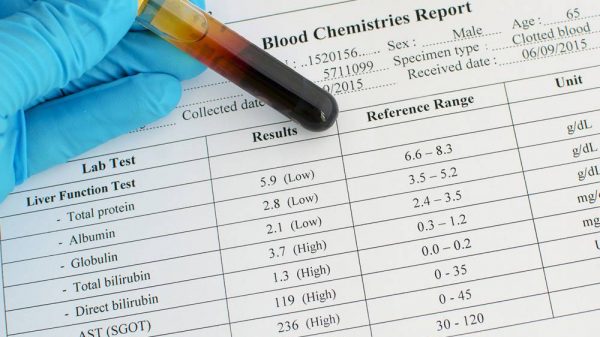
End-stage liver disease is generally regarded as irreversible and receiving a liver transplant is the best mode of treatment. The model for end-stage liver disease (MELD) allows doctors to determine how progressed the liver disease is, the probability of survival, and the need for a liver transplant. The MELD score is a measurement that takes into account bilirubin, creatinine, and rate of blood clotting.
How Do You Get Fatty Liver Disease in the First Place?
Before 1980, all cases of fatty liver disease were attributed to the overconsumption of alcohol. With the rising prevalence of fatty liver disease unrelated to alcohol, clinicians categorized NAFLD as a medical condition in 1980. (2)
Diet and lifestyle are generally regarded as the major contributors to NAFLD, but researchers have also identified genetic components that make some individuals susceptible to accumulating fat in the liver. Certain variations of the gene that codes for the PNPLA3 protein induce changes that may predispose certain people to developing fatty liver disease. PNPLA3 is an enzyme that is involved in hepatic metabolic pathways, and small alterations in the amino acids that comprise the enzyme influence whether the liver tends to accumulate fat. (3)
Furthermore, genetics plays a role in determining how fat tissue is distributed throughout the body. Some people are more likely to accumulate fat in the hips and legs. Others are prone to accumulating fat around the abdomen, which increases the likelihood of harboring fat in liver tissue.
Epidemiological research shows that a significant fraction of individuals with fatty liver disease is within a normal weight range. (4) This suggests that both the type of foods eaten and genetic propensities contribute to the development of fatty liver, regardless of body mass index.
Despite the genetic component associated with fatty liver disease, in most cases, environmental changes can help override your genetic code. In other words, even if you carry genes that predispose you to accumulate fat in your liver, you can take steps to help reverse fatty liver disease and prevent progression.
Do All Cases of Fatty Liver Disease Progress?
Interestingly, not all patients with fatty liver disease will progress.
Nonalcoholic fatty liver disease characteristically progresses slowly, with stages lasting approximately 8 years each. (5)
The risk of progressive fatty liver disease is dependent on the same factors that influence the likelihood of developing fatty liver disease in the first place.
For nonalcoholic fatty liver disease, progression is reliant upon the state of associated medical conditions. An unhealthy BMI, high blood pressure, diabetes, and insulin resistance are linked to a higher likelihood of fatty liver disease progression. These same conditions are connected to inflammation as well and exacerbate oxidative stress throughout the body. Other research shows that gut health plays an influential role in NASH. Consuming unhealthy foods alters the composition of microorganisms in the microbiome. (2) Foods high in saturated fat added sugars, and refined carbohydrates feed harmful gut flora that produces compounds that can worsen liver inflammation.
Lifestyle and dietary changes can attenuate these risk factors and reduce the probability of fatty liver disease progression.
Moreover, it turns out that genetics influence more than simply the risk of developing fatty liver disease. Your genes may also influence whether the course of fatty liver disease and your susceptibility to developing fibrosis and cirrhosis. The PNPLA3 gene, in addition to affecting the fat content of the liver, also impacts the formation of hepatic scar tissue. Certain variations of the PNPLA3 gene cause liver cells to more readily harbor fat and produce scar tissue. (2)
However, as mentioned above, your genes do not define the course of fatty liver disease. Taking the steps to follow a liver-friendly diet and lifestyle will decrease the probability of progression, regardless of whether you have the genetic tendency for fatty liver.
Life Expectancy for Fatty Liver Disease
Having fatty liver disease increases your chances of developing NASH and other liver diseases, in comparison to those without fatty liver disease. However, when you proactively respond to a NAFLD diagnosis, your life expectancy can be completely normal. While the progression of NAFLD to NASH negatively impacts prognosis and increases the probability of developing more severe liver disease, proactive response with diet and treatment of contributing conditions can restore liver health and help you maintain a normal life expectancy.
Because liver conditions are closely tied to metabolic health, NAFLD and NASH also increase the chances of developing cardiovascular disease. Mortality is the highest for those with advanced liver cirrhosis, liver cancer, and end-stage liver disease.
Are There Any Medications Available to Treat Fatty Liver?
At this time, no medications currently exist to directly treat liver inflammation and damage associated with fatty liver disease. Medications that may be useful in managing fatty liver disease are primarily used to treat metabolic syndrome. Certain drugs, such as metformin and statins, can treat associated metabolic conditions such as insulin resistance and high cholesterol. Attenuating these associated conditions, combined with weight loss and an improved diet, can help reverse fatty liver disease.
Clinical trials have shown some promise in creating drugs designed to halt inflammatory damage when fatty liver disease has progressed to NASH. There is a wide variety of drugs that aim to prevent the progression of liver damage through targeted pharmacological interventions. Some drugs specifically aim to inhibit fibrosis, while others aim to inhibit hepatic fat accumulation. Other medications are specifically designed to calm liver inflammation or block the production of harmful compounds in the gut. By 2021, medications to treat fatty liver disease are predicted to be available by prescription. (2, 6)
Should You Be Worried About Needing a Liver Transplant?
If you have just been diagnosed with early-stage fatty liver disease, a liver transplant is not the best solution. You already have a liver that’s healthy by many standards. A diagnosis of fatty liver disease serves as a warning to make changes in your diet and lifestyle that support your health.
Even if your case of fatty liver disease has progressed to NASH, a liver transplant is still a long way off. Liver inflammation is reversible. However, this doesn’t mean that you should stand by and continue your current lifestyle and diet. If you make a change to your diet and lifestyle earlier, this means your liver undergoes less damage and can more easily repair itself. The longer you wait before taking action, the longer the road to recovery, and the more likely you are to require a liver transplant down the road.
If you don’t take the necessary steps to protect your liver now, you could need a liver transplant in the future. Research shows that the number of liver transplants related to NASH has grown significantly and is predicted to become the number one cause of liver transplants in the next decade. (2)
Does Your Liver Regenerate and Is Fatty Liver Reversible?
The liver is a remarkably adaptable organ that responds to environmental changes. In fact, the liver is the only organ that can regrow following injury. Both chemical or physical injury can lead to liver damage. The liver is responsible for processing all substances that enter the body, and excessive exposure to sugar, fats, alcohol, drugs, pollutants, or other substances sends your liver into overdrive. This may cause inflammation, cellular injury, and cell death. However, when the causal factors of liver damage are removed, hepatic tissue is resilient and cells can divide to produce new, healthy hepatic cells.
The good news is at nearly every stage of fatty liver disease, there are diet and lifestyle changes that help you reverse the damage and support liver regeneration. This is why a liver transplant is the last resort for liver failure treatment. Liver transplantation is intended to treat individuals whose livers have been damaged beyond repair.
How to Reverse Liver Damage with Diet
Following a diet plan that supports fatty liver disease is critical to reversing NAFLD before it progresses. The pillars of a liver-friendly diet also help reverse associated risk factors, especially metabolic syndrome.
Here are a few tips for eating for your liver:
1. Steer Clear of Processed Foods and Refined Grains
Processed food has been altered from its original form. As a general rule, anything that is packaged has been processed. This includes granola bars, chips, crackers, cookies, etc. Processed foods usually contain loads of added sugar and preservatives, which increases your blood sugar and puts pressure on your liver to process exorbitant amounts of sugar and chemicals. Packaged meats and cheeses are also processed foods, and often contain excessive amounts of sodium and saturated fat. Refined grains like white rice, white pasta, and white bread have been processed to remove nutrients and fiber, leaving only the simple starch. Continuous consumption of processed foods contributes to liver damage and increases the risk of developing fatty liver.
2. Stay Away from Unhealthy Fats
Saturated fats and trans fats contribute not only to fatty liver disease but also to cardiovascular disease. Saturated fats can be found in many animal products, such as fatty meat, cheese, yogurt, and eggs. In general, it’s best to limit these products. When you do eat meat and cheese, make sure you stick to all-natural, unprocessed, and lean cuts of meat and low-fat, low-sodium, and low-sugar cheese and yogurts.
3. Stick to Natural, Whole, Plant-Based Foods
This means eating a variety of fruits, vegetables, whole grains, nuts, seeds, and beans. These foods contain loads of vitamins, minerals, and antioxidants that can reduce liver inflammation and promote liver repair. Plant-based foods are also rich in fiber and prebiotics that support healthy bacteria in your gut that can influence liver health.
4. Get Enough High-Quality Protein
Proteins, in many ways, are the basis of life. Amino acids are the basic units of protein and are used to carry out all biological functions. There are 20 amino acids that we need, and nine of these are characterized as essential amino acids, which means we must get them through the foods we eat. Ideal ratios of essential amino acids have been shown to support liver health. The quality of a protein source is often measured by the levels of bioavailable essential amino acids. A single meat or dairy product contains ideal ratios of amino acids. When consuming mainly plant-based foods, variation is important not only to get lots of vitamins and antioxidants but also to ensure the intake of all essential amino acids.
Conclusion
Nonalcoholic fatty liver disease is influenced by a complex of factors including diet, lifestyle, and genetic tendencies. A diagnosis of nonalcoholic fatty liver disease does not necessarily mean that the disease will progress to NASH, cirrhosis, cancer, or end-stage liver disease. Even if you have a genetic propensity for liver inflammation, diet and lifestyle play a large role in liver health. Intervening in the early stages of fatty liver disease is the key to reversing the condition so you can live a long and healthy life.
References:
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6802837/
(2) https://www.nature.com/articles/d41586-017-06926-1
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5381829/
(4) https://www.ncbi.nlm.nih.gov/pubmed/28930295