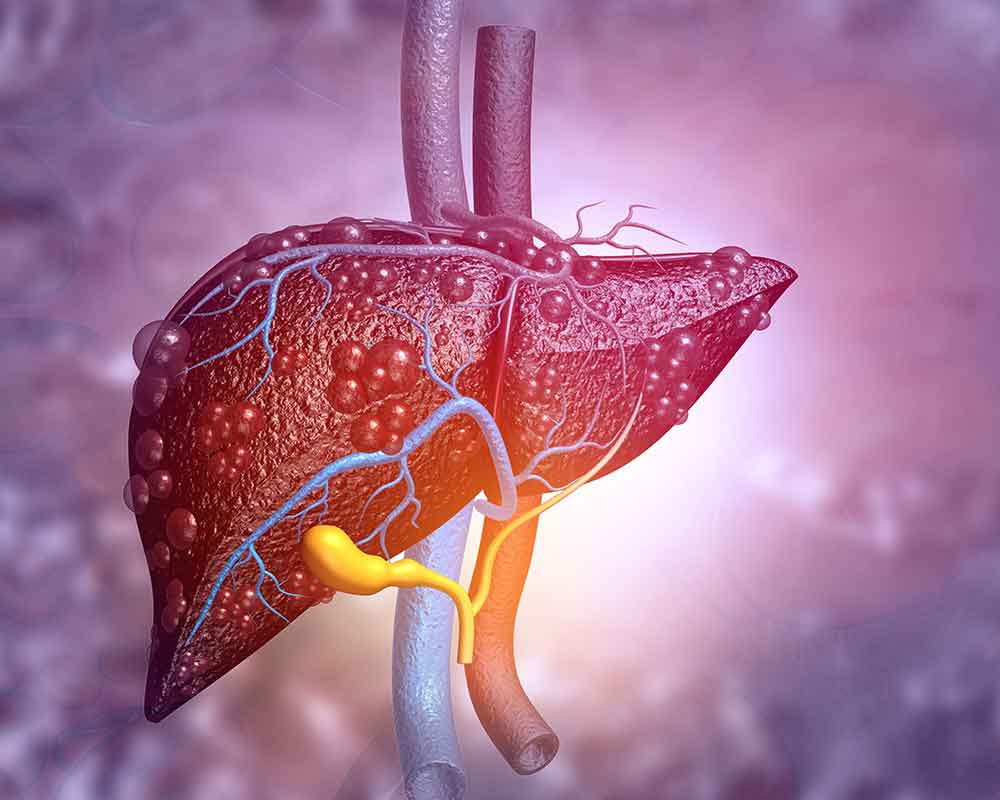
The definitive way to recognize cirrhosis is that there will be liver fibrosis, as well as nodule formation. These usually occur as a result of a chronic (long-term) injury. This, in turn, alters the normal organization of lobes in the liver. Chronic injury can occur due to many factors. Some of them include toxins, viral infections, autoimmune processes, and even hereditary conditions. Each time there is an injury, your liver heals up and fibrosis (the formation of scar tissue) occurs. This can go on for a long time while your liver retains its optimum function. But these injuries and the resulting fibrosis may build up and cause liver cirrhosis. This can either be macro-nodular or micronodular cirrhosis.
Cirrhosis will make your liver lose its proper functions. But then, the cause of cirrhosis varies, but it always starts from chronic liver disease before it progresses to cirrhosis. In developed countries, the most rampant causes of liver damage are alcohol overuse, hepatitis-C virus, and NASH. But in developing countries, the causes of liver disease are hepatitis C and B viruses. But then, Micronodular cirrhosis is often caused by too much alcohol. So it is more common in developed countries. This does not mean that people in developing countries don’t have this kind of cirrhosis, though. It only means that more people have it in developed countries than in developing countries.
What is Micronodular Cirrhosis?
There are many ways to classify cirrhosis. One of them is according to the morphology of the cirrhosis. This has three main classes:
- Micronodular cirrhosis
- Macronodular cirrhosis
- Mixed cirrhosis
This is a common classification. However, in practice, doctors use the etiologic classification more. That is more useful clinically.
Micronodular cirrhosis refers to a form of cirrhosis that has uniform nodules. The term micro connotes that these nodules usually have a diameter of less than 3mm. Micronodular cirrhosis, as we have said earlier, is often a result of too much alcohol. But it can also occur due to the following conditions:
- Hemochromatosis
- Obstruction of hepatic venous flow
- Jejunoileal bypass
- Chronic biliary obstruction
- Indian childhood cirrhosis
Macronodular cirrhosis, on the other hand, refers to cirrhosis that has irregular nodules. The nodules often have a variation higher than 3mm diameter. It can occur as a result of hepatitis C and B, primary biliary cholangitis, and deficiency in alpha-1 antitrypsin.
Mixed cirrhosis, as you may have guessed, has mixed features. There are similarities with both micronodular and macronodular cirrhosis. In many cases, micronodular cirrhosis would progress into macronodular cirrhosis with time.
Micronodular cirrhosis usually corresponds to your liver parenchyma. It is the typical “Laennec cirrhosis”, which is induced by damage from chronic alcohol overuse. But in macronodular cirrhosis, most nodules are usually larger than 3mm.
Sometimes in speaking, it is easy to confuse micronodular cirrhosis with macronodular cirrhosis since the two words sound alike. As such, many doctors refer to macronodular cirrhosis by other names. Such names include post-necrotic cirrhosis, multilobular cirrhosis, or post-hepatitic cirrhosis.
Doctors say that most cases of cirrhosis have a mixture of both micronodular and macronodular cirrhosis features. More so, the morphologic pattern often changes as the disease progresses. The nodules that start as micro-nodules have the tendency to grow larger and become macro-nodules.
This often happens when a person has alcohol-induced cirrhosis and stops alcohol intake. In short, when you remove the underlying cause of micronodular cirrhosis, the nodules are likely to grow larger.
In the case of autoimmune hepatitis, controlling necro-inflammatory activities will give rise to regenerative nodules, which are often a tad lager. But they are different from the nodules of macronodular cirrhosis.
Facts That You Should be Aware Of
Remember that the most prevalent cause of micronodular cirrhosis is an alcoholic liver disease (ALD). This often occurs progressively after many years of alcohol overuse (heavy drinking). Long-term heavy drinking causes scarring (fibrosis) in your liver. This can lead to cirrhosis in the long run.
Cirrhosis is the end-stage of ALD. However, not all heavy drinkers have ALD in the long run. One thing is sure, however. The more you drink daily and the longer you keep drinking (in years), the higher your chances of developing liver disease.
One mistake people make is that they think you can only have ALD if you get drunk often. This is not true. Your level of tolerance in terms of getting drunk has nothing to do with the chances of developing ALD.
ALD is more common in those between ages 40-50 years. But the chances are higher for men than for women. But then, women may get ALD after less alcohol exposure than men.
Experts also say there is a genetic factor in ALD and micronodular cirrhosis. It seems that some people have higher risks due to their family history.
The symptoms of cirrhosis only begin to show when advanced liver damage sets in. You are not likely to experience any symptoms when ALD begins. More often, these symptoms come on gradually.
The onset of symptoms depends on the functionality of your liver. But the symptoms are usually worse after a bout of excessive drinking.
Some of the early symptoms of cirrhosis include these:
- Fatigue and low energy
- Belly pain
- Weight loss and poor appetite
- Nausea
- Small, spider-like red marks (blood vessels) appearing on your skin
As the functionality of your liver worsens, the symptoms become more serious. Severe symptoms may include:
- The buildup of fluid in your legs (edema)
- The buildup of fluid in your belly (ascites)
- Your skin, eyes, or mucous membranes turn yellow (jaundice)
- Impotence and shrinking testicles in men
- Abnormal bleeding and easy bruising
- Confusion or cognitive problems
- Clay-colored or pale stools
How to Treat Cirrhosis
You can’t treat cirrhosis without making lifestyle changes. You will have to make certain lifestyle decisions if you want to care for your liver. Some of these include:
- Quit drinking
- Make sure to eat healthy foods and stick with a low-salt diet.
- Get the right vaccines for hepatitis, as well as for influenza and other diseases that may harm your liver.
Speak with your doctor about any drugs you will take. Do not take any herbs, supplements or over-the-counter medicines for micronodular cirrhosis without asking your doctor first. It is better not to use any drug except your doctor prescribes or approves it.