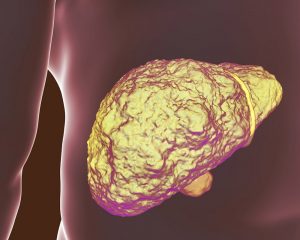
What is lung cirrhosis? Before proceeding to the pulmonary complications of cirrhosis, let us first review what it is. Cirrhosis is final-stage scarring associated with one’s liver (also known as a fibrosis). It is brought on by many types of liver disease to other conditions, such as, for example, hepatitis B or hepatitis C (most commonly), to chronic alcoholism. Each and every time the liver becomes injured, whether caused by a disease, too much alcohol intake, along with other factors, your liver attempts to repair itself. Apparent symptoms of cirrhosis associated with this illness of the liver include yellowing skin (referred to as jaundice), weakness, fatigue, appetite loss, and easily getting bruised.
When a liver is left untreated in earlier stages prior to cirrhosis, it may be more difficult to treat. Lifestyle and eating habits help alleviate this. In terms of lung cirrhosis, there are a number of primary pulmonary cirrhosis concerns in which clinicians should be more conscious of. The most frequent such concern is hepatic hydrothorax, a type of fluid accumulation when you look at the pleural space associated with portal hypertension. The other two lesser-known complications would be, one: pulmonary hypertension, and second: hepatopulmonary syndrome. Lung cirrhosis or pulmonary complications corresponding to cirrhosis are atelectasis, dyspnea, restriction with a diaphragmatic excursion (caused by massive ascites), hepatopulmonary hypoxemia, pulmonary hypertension, pleural effusion, and finally, pneumonia. Read on to learn more about cirrhosis in the lungs.
What Is Lung Cirrhosis?
How does it start? Pulmonary cirrhosis may be driven by artery pressure. It is when the pressure decreases much lower in comparison to systemic blood pressure. Your right ventricle will not necessitate muscle mass coming from your left ventricle. This will make this right ventricle more susceptible to vulnerable to problems within the environment of higher pulmonary artery pressures.
HPS is a disorder when the blood vessels dilate inside the lungs. Blood passing through the lungs is inadequately oxygenated, ultimately causing hypoxemia (a reduced oxygen level when you look at the blood) and dyspnea (difficulty breathing). The finding will be that blood oxygen levels decrease, bearing difficulty, particularly when patients move position, like lying down, sitting, and even standing–a disorder referred to as platypnea-orthodeoxia (for increased dyspnea and hypoxemia, respectively).
HPS happens to be connected with hypoxemia. It might be suspected when an individual’s pulse oximetry begins to reveal oxygen saturation at less than 97%. It would then be recommended for the patient to go through pulse oximetry with every physician visit. While an HPS occurs, pulmonary vessels start to lose their tone as they dilate. The open types of blood vessels result in surprisingly low blood pressure. Because of this, blood begins to bypass an individual’s lungs, ultimately causing hypoxia. Currently, medicine is still uncertain about why some patients suffering from cirrhosis start developing higher pulmonary artery pressures, while others experience a lower kind of pressure in the pulmonary artery. More so, there are also patients that retain normal pulmonary artery pressures. However, most patients don’t have complications such as this.
What Happens When You Have Lung Cirrhosis
During pulmonary hypertension, the obstruction or narrowing of one’s pulmonary arteries, arterioles begin to disrupt the lungs. In addition, when joined with portal hypertension, the condition would now be referred to as portopulmonary hypertension (for short, POPH). During POPH, just the right ventricle might fail when it is struggling to overcome greater pressure needed to drive blood using pulmonary circulation. Extra pressure can also be connected with a higher mortality rate of post-liver transplantation. This means that pulmonary pressure must be controlled before liver transplantation is performed on a patient.
Are There Any Symptoms?
Onset pulmonary disease can be asymptomatic, hence, clinicians should seek out proof of pulmonary disease concerning all patients that have cirrhosis. Major hepatic hydrothorax already is quite apparent during a physical check-up, and can even be confirmed right away using chest radiograph, or another imaging test like the ultrasound or through computed tomography scanning.
Additionally, cardiopulmonary complications may also be common among patients going through the final-stage kind of liver disease, making it crucial that you have pulmonary complaints evaluated if you are suffering from cirrhosis. Signs and symptoms may be a result of liver disease, but could additionally be linked to risk factors like excessive alcohol consumption, smoking, nutrition deficiency, as well as autoimmune disorders. A patient’s lung compliance may be reduced as soon as the diaphragm becomes elevated as a result of ascites plus hepatomegaly, and even also from an intrathoracic change in volume load, effusion, or atelectasis.
Additionally, deconditioning added by muscle wasting correlated to the final-stage in liver disease may aggravate dyspnea. This will lead to reduced pulmonary reserves. Patients with this may also go through an underlying chronic form of lung disease like emphysema due to chronic bronchitis, smoking, and asthma. It is just necessary that patients who are registered to go through liver transplantation give up smoking as soon as possible prior to the surgery. If not, a much higher possibility in terms of postoperative consequences like hepatic artery might occur.
Important Lung Facts
- An individual normally breathes average air at 13 pints per minute by average.
- There are two lungs in human anatomy. The right one and the left one. Combined, the two weigh about 2.9 lbs. of 1.3 kg. Your left lung and right lung do not weigh the same. In fact, the left is more light as compared to the right lung.
- Lungs can actually float. While it is not a thing many people know of, it’s a very true fact. A human being’s lungs would be the only organs within your body which carry the capacity to float while placed on water.
- Oxygen only plays a tiny part when it comes to breathing. Our air has oxygen at 21%, yet our anatomies use just 5 percent of this. The remainder becomes exhaled.
- Lungs carry taste capabilities. A study done in 2010 indicated that the human lungs come with taste receptors with the capacity of detecting exclusively bitter taste. Scientific studies revealed that anytime the taste receptors come across any type of bitter flavor, they assist the airways in relaxing. The findings became an important part of the study for the treatment of asthma.
- In spite of how much we actually exhale, it is just natural for our lungs to retain a liter of air within the airways. This is why your lungs remain the only organs in humans able to float.
This guide works just as a basic introduction to lung cirrhosis, and if you are worried about prevailing signs and symptoms, please visit a physician as soon as possible.