The detection of abnormal tissue in your liver can be frightening. The first step is to avoid panicking. Liver lesions may arise from a variety of conditions, and some of them are relatively harmless. In this article, we discuss what lesions on the liver mean, what causes liver lesions, and quick tips to improve liver health.
If you’re looking for what you need to know about liver lesions, then you’ve come to the right place. Read on to find out more.
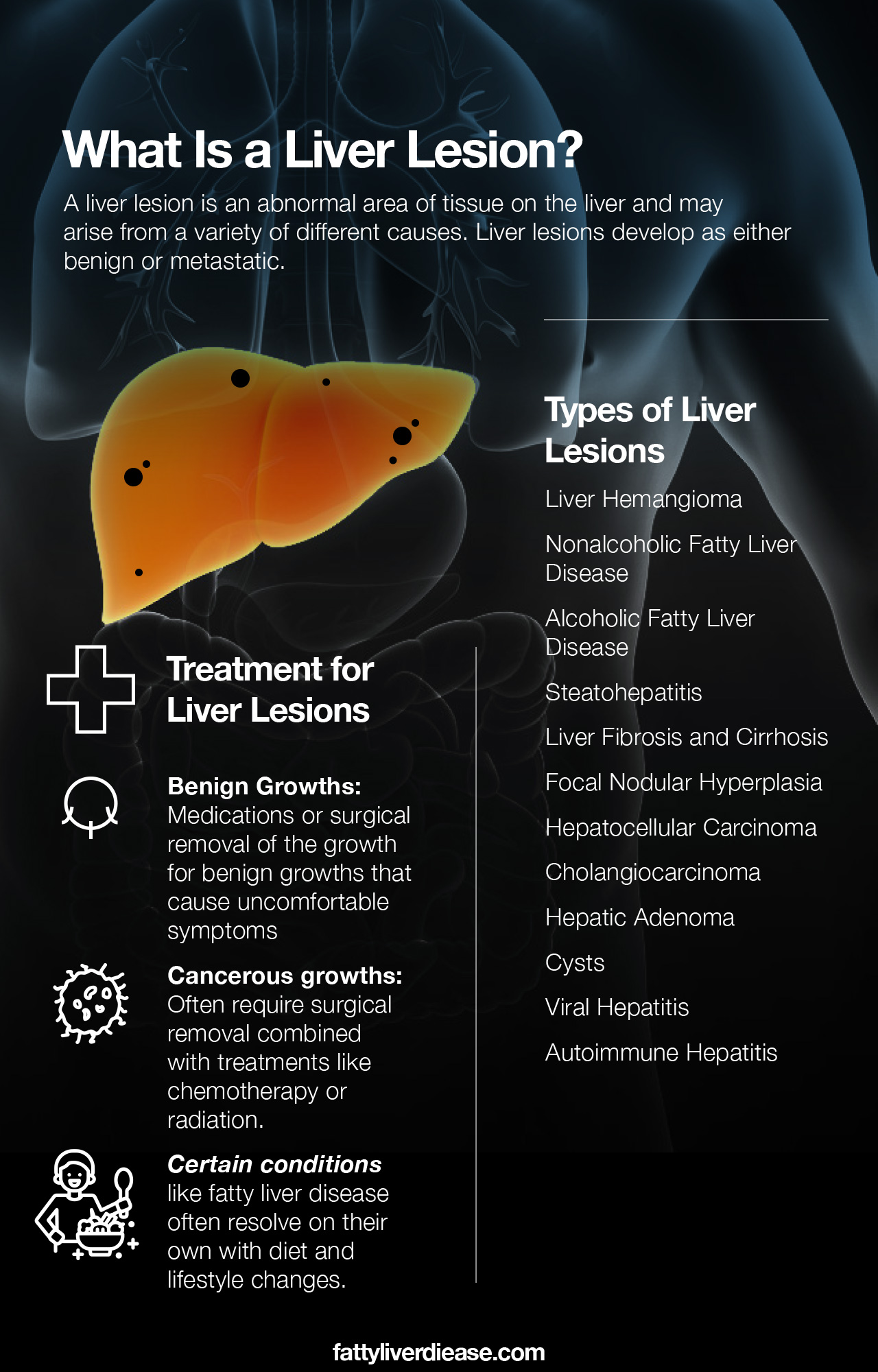
What Is a Liver Lesion?
A “lesion” is a general term that describes an abnormal area of tissue that can be found on any organ. As a result, a liver lesion may arise from a variety of different causes. Liver lesions develop as either benign or metastatic. Here we go through the different kinds of liver lesions that may develop.
Liver Hemangioma
A liver hemangioma or hepatic hemangioma is a prevalent type of liver lesion that is detected in many adults. A hemangioma is a small vascular mass that results from a cluster of blood vessels in the liver. Liver hemangiomas are generally asymptomatic, and they do not develop into liver cancer. As a result, they are described as benign liver lesions.
Less commonly, a hemangioma may cause abdominal discomfort. If an individual has multiple hemangiomas or a very large hemangioma, surgical resection may be required to remove them. A hemangioma may also be inconveniently located in the liver and impede blood flow. In this case, it’s critical to remove the mass that’s blocking blood flow.
Physicians have not determined an exact reason for why some individuals develop hemangiomas. Some individuals are actually born with hemangiomas, while others develop them later in life.
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD) has a high incidence among adults in the United States. In fact, it is estimated that nearly a quarter of American adults have fatty liver disease. The characterization of NAFLD includes the intrahepatic collection of fat within hepatocytes, or liver cells. This means that instead of accumulating around liver cells, small fat particles make their way inside liver cells.
Though a genetic component may contribute to NAFLD, this liver condition is often associated with a diet high in added sugars and saturated fat. The chances of developing NAFLD is also higher for individuals who have risk factors like obesity, type 2 diabetes, and insulin resistance.
Alcoholic Fatty Liver Disease
Like NAFLD, alcoholic fatty liver disease is characterized by the accumulation of fat particles within the liver. However, instead of being caused by a poor diet, alcoholic fatty liver disease results from chronic alcohol abuse. Over time, excess alcohol consumption can lead to the development of liver lesions characteristic of alcoholic fatty liver disease.
Steatohepatitis
Steatohepatitis is an inflammatory condition resulting from untreated NAFLD or alcoholic fatty liver disease. Continued fat accumulation in the liver irritates liver cells and can cause inflammation. Chronic inflammation characterizes steatohepatitis. When fatty liver disease has progressed to steatohepatitis, the chances of developing liver fibrosis and liver cirrhosis increase significantly. Chronic inflammation also increases the risk of developing liver lesions.
Liver Fibrosis and Cirrhosis
Liver fibrosis is a process that causes the production of rigid, collagen-like material in the liver. Fibrosis occurs as the next step in liver disease progression, following fatty liver disease and steatohepatitis. Continued inflammation that results from steatohepatitis causes damage that the body handles by producing scar tissue. Over time, ongoing fibrosis leads to a condition called liver cirrhosis.
A cirrhotic liver may be so scarred that it becomes hard in texture, compromising liver function. If liver cirrhosis affects too much liver tissue, it can eventually lead to liver failure. Liver cirrhosis also increases the risk of developing liver cancer.
Focal Nodular Hyperplasia
Focal nodular hyperplasia (FNH) is relatively uncommon. FNH is a non-cancerous or benign hepatic tumor that develops in the liver. These focal liver lesions or nodules generally cause no symptoms and seem to be linked to birth control pills. They are linked to a central scar on image tests. Unless they are causing symptoms, FNH may also not require any treatment.
Hepatocellular Carcinoma
Though more rare, hepatocellular carcinoma (HCC) can be a cause of liver lesions. Hepatocellular carcinoma is the medical term for liver cancer. Individuals who have experienced chronic liver inflammation and damage tend to be at the highest risk for developing liver cancer. Chronic and advanced conditions like steatohepatitis, viral hepatitis, fibrosis, and cirrhosis cause substantial inflammation that interferes with the normal function and DNA code of liver cells. As a result, cancerous cells develop, and the immune system fails to induce apoptosis (also known as cell death). Cancerous cells then flourish and form growths that seriously interfere with liver function and spread to other organs.
A diagnosis of HCC means you will likely need to undergo aggressive cancer treatment. Liver cancer may spread to other organs, meaning it metastasizes to other areas of the body or becomes metastatic cancer.
Liver cancer can also be the result of liver metastases. If you have liver metastases, this means that liver cancer has spread from another area of the body. There are several cancers that tend to spread or metastasize to the liver. For example, cancer may spread from the pancreas, breast, kidney, and esophagus.
Cholangiocarcinoma
Cholangiocarcinoma is a type of hepatobiliary cancer that specifically impacts the biliary ducts. The bile ducts are essential in the body because they carry bile from the liver to the gallbladder and ultimately to the small intestine. There is an extensive network of bile ducts, and cholangioma will be diagnosed depending on the placement of cancerous growths in the bile ducts. These three types are called distal, perihilar, and intrahepatic cholangiocarcinomas.
In particular, intrahepatic cholangiocarcinoma is the type of bile duct cancer that develops within the liver. As a result, individuals with this type of cancer may develop liver lesions.
Hepatic Adenoma
A hepatic adenoma or hepatocellular adenoma is a form of liver tumor that is benign. Hepatic adenomas are very rare and tend to be connected to hormone levels, particularly estrogen. For that reason, they tend to be linked to the use of oral contraceptives. These growths may sometimes be connected to liver hemorrhages.
Cysts
Like most kinds of liver lesions, liver cysts are generally benign, so they don’t cause cancer. Cysts may be filled with fluid, or they may be solid in texture. Cysts usually cause no symptoms. Very seldomly, cysts may cause belly pain in the upper right quadrant of the abdomen. If an individual develops uncomfortable and persistent symptoms, undergoing surgery to remove the cyst may be the recommended course of action.
Another cystic growth can develop, referred to as a cystic tumor. The majority of these are also benign and are referred to as cystadenomas. However, it is possible for the cystic tumor to undergo a malignant transformation to become malignant lesions, though this tends to be more rare.
Viral Hepatitis
Viral infection causes viral hepatitis. There are many types of hepatitis such as hepatitis A, hepatitis B, and hepatitis C. However, hepatitis C is the most common type of hepatitis in the United States. Hepatitis C is usually contracted through contact with contaminated blood or through sexual contact.
An individual may have hepatitis for many years without symptoms, making it easy for the virus to go undetected. Over time, unresolved hepatitis C can cause inflammation and liver lesions. Historically, hepatitis C had no cure. Luckily, today, hepatitis C can be successfully treated with antiviral drugs.
Autoimmune Hepatitis
Autoimmune hepatitis is a form of autoimmune disease that attacks the liver. Autoimmune diseases are characterized by an immune system that attacks healthy tissue. In the case of autoimmune hepatitis, the immune system malfunctions and recognizes healthy liver tissue as a threat to the body. As a result, the immune system launches attacks on the liver to kill the healthy tissue mistaken for foreign invaders.
Constant attacks from the immune system cause autoimmune hepatitis, which is chronic inflammation. Over time, this inflammation may give rise to liver lesions.
Detecting Liver Lesions and Diagnosis
A physician will evaluate your symptoms and order tests to determine whether you have liver lesions.
Possible Signs and Symptoms
A physician may expect the presence of liver lesions due to other indicators. Symptoms like jaundice or yellowing of the skin, fatigue, unexpected weight loss, and abdominal pain may indicate the presence of liver disease.
Your physician may also order tests to examine the levels of liver enzymes in your blood. Blood tests may measure levels of AST and ALT. Elevated liver enzymes mean that your liver is more inflamed than it should be.
Your doctor may also be able to detect liver abnormalities by using a technique called palpation. During palpation, a doctor can manually feel the liver and detect enlargement or, sometimes, the presence of growths.
It’s important to keep in mind that you may have no symptoms of liver disease or liver lesions. Harmless or benign liver lesions also cause no symptoms and can only be detected by imaging technology.
Imaging Techniques
Liver lesions are almost exclusively detected by medical imaging techniques. Several different types of imaging studies can reveal the presence of liver lesions. Ultrasound technology or ultrasonography uses sound waves to produce sound waves that create an image of the organ. Depending on the texture and density of liver tissue and lesions, the sound waves will differ and depict the presence of abnormalities. For example, if you have a higher than normal fat content in your liver, the ultrasound will reveal a higher echogenicity, meaning sound waves bounce off the fat tissue more readily.
Computed tomography (CT scans) and magnetic resonance imaging (MRI) are other imaging types that can also yield information about the health of your liver tissue. Arterial phase enhancement may be useful in both types of imaging to reveal more details about liver health. MRI imaging tests are often performed using contrast, which allows for an even more accurate and detailed image of your liver to be revealed. Your physician will be able to recommend the best imaging modality for your specific needs.
Imaging will help physicians make a differential diagnosis, which narrows down the possible causes to a few possibilities. To confirm exactly what is causing the abnormalities, your physician will likely recommend a biopsy. A biopsy entails removing a small sample of the liver and subjecting it to analysis with a microscope. Medical professionals will be able to determine whether the liver cells look normal under the microscope, or whether there is an abnormality that requires attention. A liver biopsy will also be able to yield specific information about the cause of the liver lesion.
Medical imaging tests for your liver lesions are conducted and interpreted by specialists in the field of radiology. Depending on the results and your case of liver lesions, you will then be referred to specialists for treatment and evaluation.
Should I Be Worried About Liver Lesions?
It’s important not to worry too much about liver lesions until their cause is confirmed by your doctor. Malignancy tends to be rare in hepatic lesions. The majority of liver lesions are not cancerous, so it’s important not to panic until a biopsy is performed and the cells are analyzed by a physician.
Treatment for Liver Lesions
The treatment for liver lesions will depend on the root cause of the lesions. Always follow medical treatments and advice and discuss all at-home remedies with your physician.
For benign growths that cause uncomfortable symptoms, your doctor will likely recommend medications or surgical removal of the growth to ease symptoms.
Cancerous growths will often require surgical removal combined with treatments like chemotherapy or radiation.
Benign growths that cause no symptoms may not require any treatment at all. On the other end of the spectrum, extremely advanced liver disease with serious liver lesions may result in end-stage liver failure, which is most successfully treated with a liver transplant.
Certain conditions like fatty liver disease often resolve on their own with diet and lifestyle changes.
Things You Can Do to Support Your Liver
Regardless of whether you have liver lesions, it’s a good idea to take care of your liver. The liver is a vital organ that we simply cannot live without!
1. Cut Back on Alcohol
If you are in the early stages of alcoholic fatty liver disease, quitting drinking is the best thing you can do for your liver. Drinking excessive amounts of alcohol increases the risk of developing alcoholic fatty liver disease, steatohepatitis, fibrosis, and cirrhosis. However, cutting alcohol out of your lifestyle can entirely reverse the early stages of alcoholic fatty liver disease.
Even if you don’t have alcoholic fatty liver disease, cutting back on alcohol consumption and limiting your alcohol moderation. Keep in mind that the liver is responsible for processing and detoxifying all of the alcohol we consume. Metabolizing alcohol takes a toll on liver tissue, causing the buildup of reactive oxygen species called free radicals. Excessive free radicals can accumulate and cause oxidative and inflammation over time, increasing the risk of developing liver diseases and even liver cancer.
In other cases, cutting alcohol out of your lifestyle can reduce inflammation in the liver and help your liver heal from other inflammatory conditions.
2. Clean Up Your Diet
Eating a healthy diet rich in fruits, veggies, whole grains, nuts, seeds, and fatty fish can help protect liver health. These whole-foods are packed with anti-inflammatory ingredients and antioxidants that help protect the liver from damage while also helping repair inflicted damage. Eating a healthy diet is also critical for metabolic health and reversing NAFLD.
Fruits and vegetables contain an abundance of antioxidants like polyphenols and carotenoids that help neutralize free radicals. This helps protect the liver from toxins while helping it repair from damage and inflammation. Incorporate fruits and vegetables into your diet by choosing foods like kale, spinach, tomato, lettuce, arugula, apples, blueberries, raspberries, and persimmons.
Whole grains are crucial for liver health because they offer not only vitamins and minerals but also lots of fiber. Eating lots of fiber is important for supporting both gastrointestinal health and liver health. And surprisingly, these two organ systems are uniquely connected.
3. Avoid Smoking
Smoking introduces tons of chemicals into the body via the lungs. Chemicals are absorbed through the lungs and into the bloodstream, where they can then travel to the liver and cause inflammation and damage. Smoking also negatively impacts blood pressure and cardiovascular health. If you are dependent on cigarettes, talk to your doctor about options that help you quit smoking.
4. Exercise Caution with Certain Medications and Chemicals
Remember, the liver must process everything we put in our body, including medications and chemicals we ingest. Always make sure that you use medications as directed since some can cause liver damage if taken in excess.
5. Attend Regular Check-Ups
It’s important to keep up with your yearly physicals, to make sure that your health is in good shape. Because some liver diseases have no symptoms, it’s a good idea to check in with your doctor each year. A physical exam and blood tests will help reveal if you may be developing liver disease or if you are at risk of developing it.
If you have a liver lesion that is not benign, catching liver disease early is key to a successful treatment. You will likely see experts in hepatology, radiology, gastroenterology, and internal medicine when receiving treatment for a liver mass or chronic liver disease.
It’s also crucial to attend all follow-up appointments as you are undergoing treatment, to be sure that you are responding as expected.
What It Means to Have Liver Lesions: Final Words
Liver lesions are most commonly benign and arise as cysts or other small masses of tissue. Many of these benign lesions don’t cause symptoms and don’t require treatment. There are numerous liver lesions causes. Liver lesions may be a result of liver diseases like viral hepatitis, fatty liver disease, and autoimmune hepatitis. A very small fraction of liver lesions are cancerous and require intensive treatment. In any case, it’s crucial to take care of your liver to make sure it remains as healthy as possible. Be sure to limit your alcohol intake, eat a balanced diet, and attend yearly physicals.