Being pregnant is already difficult without the added complications linked with carrying another human being for the next nine (9) months. However, challenges can and will occur during this very tender stage of a woman’s life. Some may experience physical issues such as weight gain and changes to the blood pressure, while some may experience mood swings and distress caused by hormonal changes. One other thing that may get pregnant women worried is jaundice during their pregnancy. But what causes jaundice during pregnancy? What are the possible protective and fetal outcomes? In this article, we answer the said questions and if you want to know more, then read on!
Jaundice During Pregnancy: A General Overview
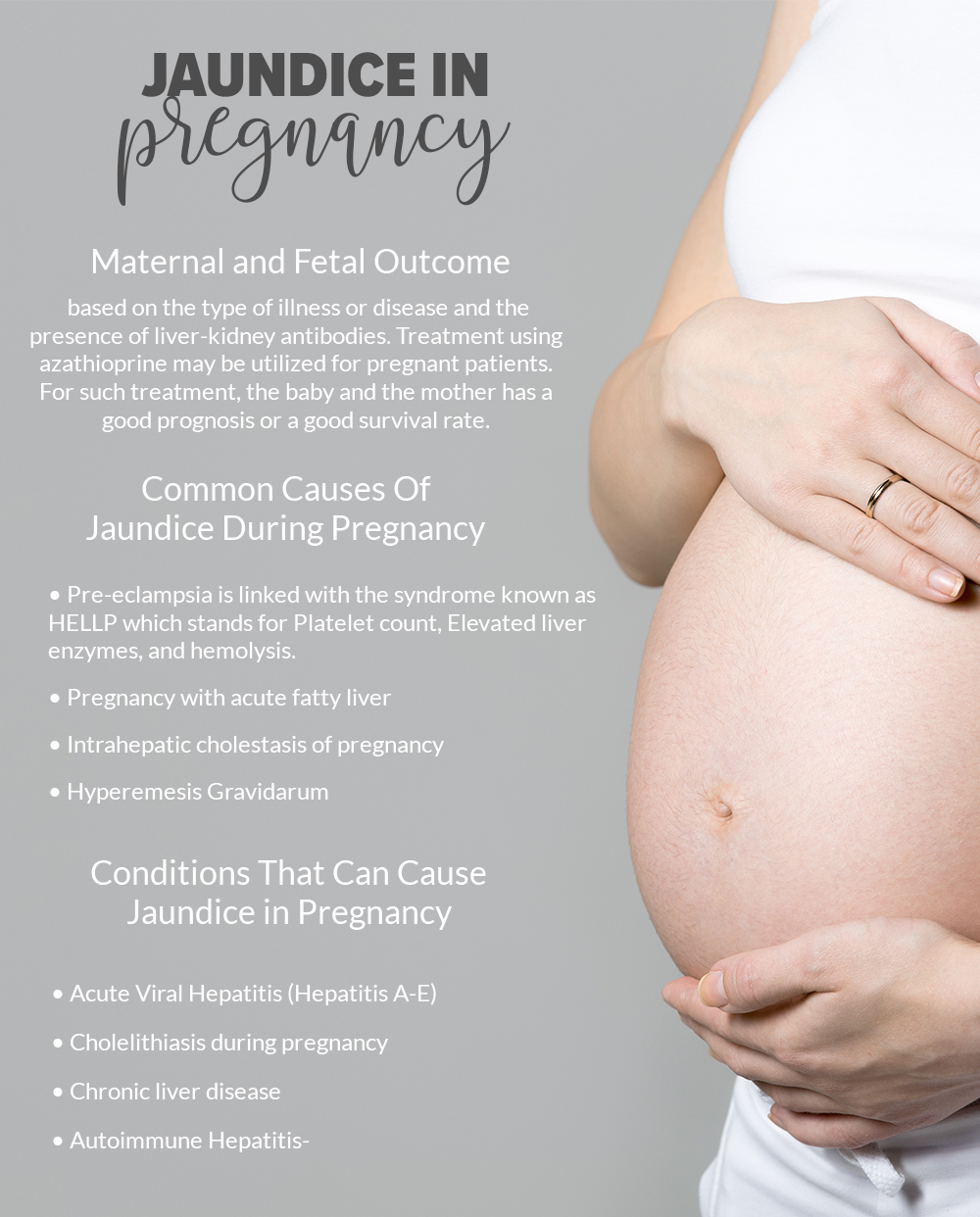
While it can be rare to experience jaundice during pregnancy, it is a medical condition that can occur. This condition can be an indicator of something very risky for both the mother and the unborn child. It can occur intercurrently or it may be caused by the pregnancy itself. Some of the more common causes of jaundice during pregnancy include the following:
- Pre-eclampsia linked with the syndrome known as HELLP which stands for Platelet count, Elevated liver enzymes, and hemolysis.
- Pregnancy with acute fatty liver
- Intrahepatic cholestasis of pregnancy
- Hyperemesis Gravidarum
Some of the clinical features that are presented in liver disease during pregnancy can commonly be nonspecific and will have symptoms such as abdominal pain, vomiting, nausea, and jaundice. All diseases of the liver that occur while pregnant can result in increased fetal and maternal mortality and morbidity.
Conditions That Can Cause Jaundice in Pregnancy
Below are some of the possible conditions that can lead to jaundice during pregnancy
1. Acute Viral Hepatitis
One of the most common causes of jaundice during pregnancy is viral hepatitis with infections caused by viruses from hepatitis E, hepatitis D, hepatitis C, hepatitis B, and hepatitis A. Hepatitis incidence during pregnancy can vary immensely across the globe. In countries that hepatitis incidence is at 0.1% while in countries that are just developing it can move up much higher (around 3% to 20% more). Most cases of infections caused by the hepatitis virus do not cause any significant adverse alterations to the pregnancy except for hepatitis E which can lead to rates of fatality amounting to 10% to 20%. Some of the things that individuals can do for different hepatitis strains include:
a. Hepatitis A
- Have the patient that is infected isolated
- Treatment that is symptomatic can have treatments such as maintenance of nutrition and hydration.
- Women who are pregnant who come into contact with the hepatitis A virus can be provided with immune globulin within half a month of being exposed along with some vaccination.
- It is still not certain if virus transmission can occur from the mother to the infant but it is recommended that the newborn be given immune globulin if hepatitis A occurred during the final month of being pregnant.
b. Hepatitis B
- Hepatitis B is one of the most common acute viral hepatitis causes and can present itself in chronic, subclinical, and acute forms.
- HBeAg’s presence is linked with an increased risk of infection for neonates.
- Female patients are all provided with the option to have a screening for hepatitis B as part of routine screening during the antenatal phase.
- Women with infants who are positive for HBeAg should be provided with immunoglobulin of hepatitis B at birth and after a week, a vaccine for hepatitis B should be administered. This procedure can reduce the vertical transmission of hepatitis B to lower than 3%.
- The infection of the newly born will be dependent as to when the infection occurs during gestation.
c. Hepatitis C
- There is currently no therapy available that can positively influence hepatitis C virus transmission.
- The medication known as interferon should be avoided while the individual is pregnant as it can adversely affect the fetus.
d. Hepatitis D
- Hepatitis D can occur as part of a hepatitis B infection. Once this occurs, it can lead to an increased incidence of acute failure of the liver.
e. Hepatitis E
- While this form of hepatitis can be rare in more developed countries, it can cause liver failure and high death rates for women in underdeveloped and developing countries.
- For example, hepatitis E can lead to higher rates of maternal mortality in India compared to other forms of hepatitis that are acute during pregnancy.
2. Cholelithiasis during pregnancy
Gallstone disease that is symptomatic is second to the most common emergency of the abdomen for women who are pregnant. This condition is estimated to affect only 6% of women who are pregnant and out of this, only one out of 20 can actually get jaundice. Being pregnant can lead to the alteration of the composition of the bile and a slow down in gallbladder emptying which can lead to increased gallstone risk particularly during the second trimester of pregnancy.
Some of the symptoms of this medical condition include pain in the epigastrium or upper right quadrant which can peak at around 12 hours to one whole day. Another possible symptom is that there can be pain that can radiate toward the back and tenderness in the upper right quadrant. Jaundice caused by obstructions such as gallstones will require intervention via a surgical procedure. Fetal loss is pegged at around six percent.
3. Chronic Liver Disease
Those with chronic liver disease can have a fetal loss at increased rates or levels.
- Patients suffering from PBC or primary biliary cirrhosis should be warned that the said medical condition (PBC) can lead to worsened symptoms of cholestasis.
- Patients whose infants have significant hyperbilirubinemia may need to undergo an exchange transfusion after being born.
4. Autoimmune Hepatitis
This kind of hepatitis can have an attack that is acute. Bilirubin serum may have increased levels during this period based on the type of illness or disease and the presence of liver-kidney antibodies. Treatment using azathioprine may be utilized for pregnant patients. For such treatment, the baby and the mother has a good prognosis or a good survival rate.