Rheumatoid arthritis is a condition that affects the joints of many Americans. Getting a diagnosis of rheumatoid arthritis can be confusing and leave you with many questions. Is rheumatoid arthritis genetic? Is it reversible? Here we go over everything you need to know about rheumatoid arthritis to allow you to maintain a high quality of life and continue completing daily activities.
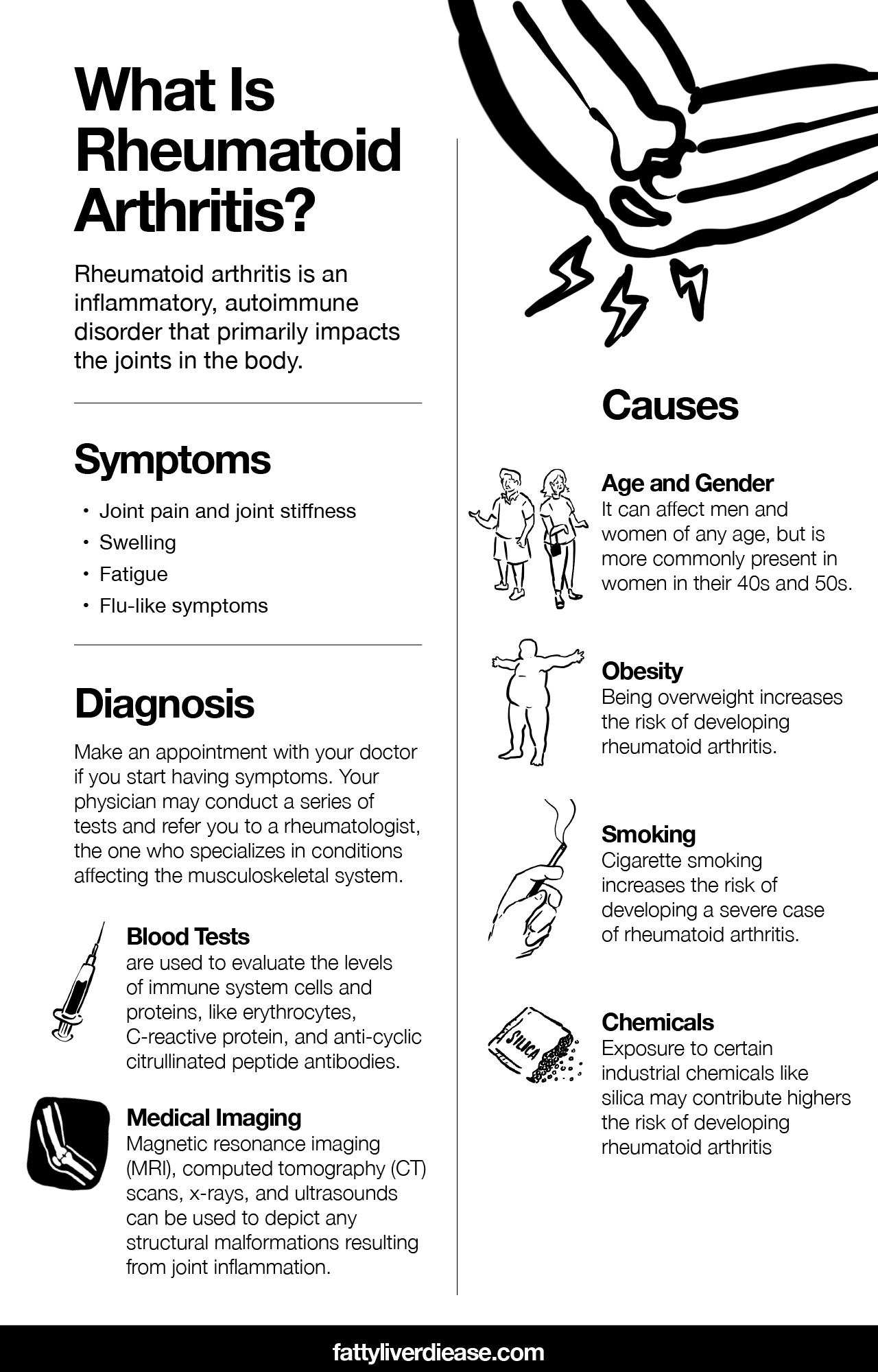
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is an inflammatory, autoimmune disorder that primarily impacts the joints in the body. It is a chronic disease that if left untreated, can lead to severe joint damage. Though there are several different types of arthritis, rheumatoid arthritis describes a form that results from immune system dysfunction.
To better understand rheumatoid arthritis, let’s break down the meanings of “inflammation” and “autoimmune.” Inflammation and autoimmunity share a closely related, causal relationship. A state of inflammation indicates immune system hyperactivity. If the immune system is hyperactive, this means that it reacts to circumstances that it shouldn’t be reacting to. Normally, the immune system is triggered to attack foreign invaders like viruses and bacteria or deformed cells that could lead to tumors or cancer. However, in a state of inflammation, the immune system reacts to any small trigger.
Autoimmunity develops when the hypersensitive immune system is activated in response to normal body tissues. In essence, the body begins launching immune system attacks against itself. This may mean that the immune system targets the nervous system, digestive system, liver, or really any body system.
Rheumatoid arthritis is a form of inflammatory arthritis that results in chronic inflammation in the joints. The immune system malfunctions and targets the delicate tissues lining the joints called the synovium. Inflammation damages the synovium over time, which can also lead to damaged bone, cartilage, and tendons.
Inflammation and autoimmunity are associated with numerous non-communicable conditions like insulin resistance, type 2 diabetes, obesity, fatty liver disease, lupus, and multiple sclerosis.
Symptoms of Rheumatoid Arthritis
If you’ve been struggling with rheumatoid arthritis, then you have likely experienced some pretty uncomfortable and painful symptoms.
The most typical presentation of rheumatoid arthritis includes:
- Joint pain and joint stiffness: Typically, stiffness will be felt in the joints, particularly in the larger joints of the fingers and toes. Stiffness tends to be the worst in the morning and gradually improves as the day progresses.
- Swelling: Finger and toe joints may appear to be swollen and misshapen.
- Fatigue: Because rheumatoid arthritis is an inflammatory condition, symptoms are not always restricted to the joints. Inflammation can be systemic, causing fatigue and exhaustion.
- Flu-like symptoms: It’s not uncommon for rheumatoid arthritis to also be accompanied by fever, chills, and body aches. In the case of rheumatoid arthritis, these symptoms are the result of systemic inflammation that irritates body tissues and causes more generalized symptoms.
Rheumatoid arthritis often exhibits in a pattern characterized by flare-ups that then resolve. Flare-ups can best be described as periods of time when the individual experiences more symptoms as a result of increased disease activity. While the above-listed symptoms are typical, rheumatoid arthritis can also have an atypical presentation. More unusual symptoms of rheumatoid arthritis impact other areas of the body, such as the skin, eyes, lungs, heart, and kidneys.
How Is Rheumatoid Arthritis Diagnosed?
If you start having symptoms of rheumatoid arthritis, it’s a good idea to make an appointment with your doctor. A physician will be able to evaluate your symptoms to make the proper diagnosis. Your physician may conduct a series of tests and refer you to a rheumatologist, which is a physician who specializes in conditions affecting the musculoskeletal system.
Tests are the most conclusive way to determine whether your symptoms are the result of rheumatoid arthritis. Blood tests are used to evaluate the levels of immune system cells and proteins, like erythrocytes, C-reactive protein, and anti-cyclic citrullinated peptide antibodies. Elevated levels of these particles indicate high levels of inflammation throughout the body that are characteristic of rheumatoid arthritis.
In addition to blood tests, medical imaging is a useful tool for diagnosing rheumatoid arthritis. Magnetic resonance imaging (MRI), computed tomography (CT) scans, x-rays, and ultrasounds can be used to depict any structural malformations resulting from joint inflammation.
Causes: Is Rheumatoid Arthritis Hereditary or Environmental?
The exact cause of rheumatoid arthritis is largely unknown. When determining the cause of a condition, it’s important to examine whether genetic or environmental factors play a greater role.
Is rheumatoid arthritis genetic? The risk of rheumatoid arthritis may in part be due to genetic factors. Medical professionals believe that genetics may play a small role in the risk of developing rheumatoid arthritis. As is the case with many diseases, a family history of rheumatoid arthritis seems to be associated with an increased risk of developing the condition. For example, if your parents developed rheumatoid arthritis, you may have a slightly higher likelihood of developing the disease as well. However, overall, physicians and researchers agree that environmental and other risk factors play a greater role in the development of rheumatoid arthritis than do genetic risk factors.
While the cause of rheumatoid arthritis has yet to be identified, there are certain risk factors associated with the development of the condition. Most are associated with environmental causes. Rheumatoid arthritis risk factors include: (1)
- Age and gender: Though rheumatoid arthritis can affect men and women of any age, it tends to more commonly present in women in their 40s and 50s.
- Obesity: Being overweight increases the risk of developing rheumatoid arthritis, potentially because carrying excess weight is connected to higher levels of systemic inflammation.
- Smoking: Cigarette smoking increases the risk of developing a severe case of rheumatoid arthritis.
- Chemicals: Exposure to certain industrial chemicals like silica may contribute to the risk of developing rheumatoid arthritis.
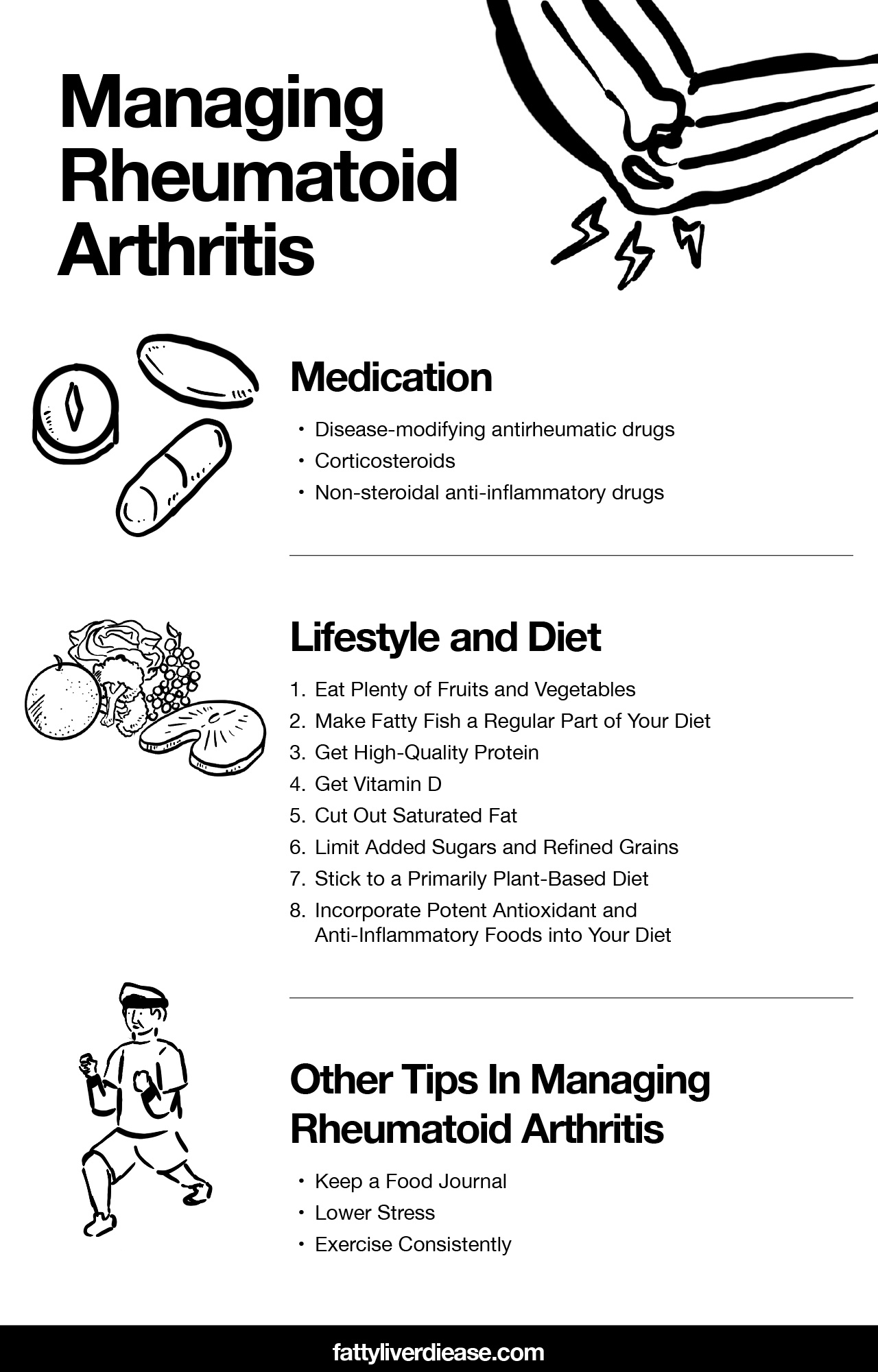
Treating Rheumatoid Arthritis
Though no cure currently exists for rheumatoid arthritis, there are medications and lifestyle changes that can help you manage symptoms and keep arthritis flare-ups at a minimum.
Managing Rheumatoid Arthritis with Medications
Several types of medications help manage the symptoms of rheumatoid arthritis and enhance the quality of life.
- Disease-modifying antirheumatic drugs: These immunosuppressant medications, known as DMARDs, work by decreasing immune system activity. As a result, the immune system is largely unable to continue launching attacks against the body. Because DMARDs address the root cause of rheumatoid arthritis, they are generally used to control the disease for a long period of time.
- Corticosteroids: Medications like prednisone are useful for quickly relieving inflammatory symptoms associated with rheumatoid arthritis. Unlike DMARDs, they are not usually appropriate to use over a long period of time.
- Non-steroidal anti-inflammatory drugs: Also known as NSAIDs, these medications help decrease joint inflammation and relieve associated swelling and pain. You can purchase NSAIDs over-the-counter, though prescription NSAIDs are also available.
Things to Keep in Mind
Make sure to discuss all of your medical conditions with your physician before starting certain medications. Some medications can be associated with negative health outcomes. In particular, long-term use of DMARDs may increase the risk of developing liver problems. Your physician will closely monitor your health to make sure that you’re responding positively to all medications.
Managing Rheumatoid Arthritis with Lifestyle and Diet
When used alongside a medical treatment plan, lifestyle and diet changes can be a crucial part of decreasing the frequency of arthritis flare-ups and managing symptoms. Here are some tips for making lifestyle and diet changes that support relief from rheumatoid arthritis symptoms.
1. Eat Plenty of Fruits and Vegetables
Fruits and vegetables are some of nature’s most potent healing foods. Eating an abundance of fruits and vegetables helps to support a healthy immune response. Fruits and veggies are filled with micronutrients like vitamins, minerals, and antioxidants that help the cells throughout your body function as efficiently as possible.
2. Make Fatty Fish a Regular Part of Your Diet
Why is fatty fish good for you? Because it’s packed with healthy fats called omega-3 fatty acids. Omega-3 fatty acids are a type of polyunsaturated fat that helps improve the immune system response and lower inflammation throughout the body. Omega-3 fatty acids have been shown to be effective for supporting healing for a variety of other diseases, including fatty liver disease and type 2 diabetes. Fish that are particularly rich in omega-3 fatty acids include salmon, mackerel, sardines, and Arctic char.
Having trouble incorporating fish into your diet on a regular basis? Supplements can make up for that. Just make sure you find a high-quality supplement that provides pure fish oil so that you’re not intaking a lot of additives and impurities.
If you follow a plant-based diet, you can also find plant forms of omega-3 fatty acids in foods like flaxseeds, chia seeds, walnuts, and pecans.
3. Get High-Quality Protein
Getting enough protein is crucial for numerous biological functions. The biologically useful part of protein is nitrogenous compounds called amino acids, which are strung together in patterns to obtain a protein structure. When we eat protein, the digestive system breaks protein down into its individual amino acids. Nutritional protein offers two kinds of amino acids: essential and nonessential amino acids. The essential amino acids are the ones that we must consume in optimal ratios on a daily basis, in order to support ideal health and functioning. The body is unable to produce essential amino acids, and they must be obtained from dietary sources. On the other hand, we can do without nonessential amino acids on a daily basis simply because the body is able to manufacture them on its own.
Getting balanced ratios of essential amino acids on a daily basis supports healthy immune system function as well as the synthesis of muscle and connective tissue. Healthy immune response and muscle connective tissue synthesis help fight against rheumatoid arthritis. making sure that you get balanced ratios of essential amino acids in your diet helps ensure that the immune system is equipped and has enough raw materials to react appropriately to triggers.
On top of that, having the raw materials necessary for muscle and collagen synthesis helps patients with rheumatoid arthritis maintain their strength. Many patients with rheumatoid arthritis have difficulty with certain movements, feel fatigued, and are unmotivated to engage in exercise during flare-ups. As a result, individuals with rheumatoid arthritis may be more prone to muscle wasting, which contributes to loss of strength. As discussed above the autoimmunity attacking the lining of the joints can also extend to breakdown and damage of the collagen and connective tissue within and surrounding the joints. Consuming a balanced ratio of essential amino acids supports your body in maintaining and rebuilding muscle, collagen, and connective tissue in these areas. Without adequate support for your muscles and connective tissue, it will be easier for your body to maintain strength through a flare-up.
So, where can you get balanced ratios of essential amino acids? Animal proteins contain optimal ratios of the essential amino acids in a single source. However, to keep inflammation at a minimum it’s important to limit most animal products, when choosing to consume animal products, stick to low-fat and nonfat options likes Greek yogurt, chicken breast, and turkey breast. For an individual with rheumatoid arthritis, the best source of essential amino acids is salmon, since it contains high-quality protein but also anti-inflammatory omega-3 fatty acids.
Keep in mind that if you follow a primarily plant-based diet, it is still possible to make sure that you’re getting all the essential amino acids that you need. the only catch is that you must incorporate several plant-based sources of essential amino acids into your diet on a daily basis, to ensure that your body is getting optimal ratios of all essential amino acids. Vegetable sources of essential amino acids include tofu, tempeh, soybeans, walnuts, almonds, peanuts, and beans.
4. Get Vitamin D
Research shows that vitamin D deficiency is very common among individuals with rheumatoid arthritis. (2)
Vitamin D is a powerful regulator of the immune system, and plays a role in lowering inflammation and making sure that immune responses are appropriate. If you’ve been diagnosed with rheumatoid arthritis, it is worth asking your physician to test your vitamin D levels.
Making sure that you get enough vitamin D may help prevent arthritis flare-ups and improve the severity of your symptoms. Where can you get the vitamin D you need to ward off flare-ups? Yet this crucial vitamin through your diet. However, vitamin D is naturally present in very few foods. One of the richest natural sources of vitamin D is mackerel. mackerel is also rich in omega-3 fatty acids. Though not quite as concentrated in vitamin D, salmon is another great choice that also affords omega-3 fatty acids. luckily there are also many foods that are fortified in vitamin D such as yogurt, milk, soy milk, and orange juice.
Though certain foods are fortified with vitamin D, it is still extremely difficult to get sufficient amounts of vitamin D in your diet to fight against and prevent autoimmune disease. Getting exposure to the sun is an excellent way to boost vitamin D synthesis in your skin. An individual with light skin can synthesize sufficient amounts of vitamin D after just 10 to 15 minutes of sun exposure. an individual with darker skin may need up to an hour of sun exposure to synthesize the same amount of vitamin D. Either way, getting sun exposure is an extremely effective way to boost your vitamin D levels. just be cautious not to get burned and to always protect your skin from overexposure.
Finally, if you’re living in a cooler climate and/or you eat a primarily plant-based diet, we can be nearly impossible to obtain enough vitamin D to prevent and manage autoimmune conditions like rheumatoid arthritis. In these cases, supplementation is the best option. Choose vitamin D3 supplements and aim to take up to 5000 IU on a daily basis. Vitamin D is more readily absorbed when taken with calcium and magnesium supplements.
5. Cut Out Saturated Fat
Saturated fat is a major cause of inflammation in the American diet. Saturated fat can be found in numerous food sources like whole milk, steak, pork, and nearly all whole animal products. Saturated fat, consumed through the diet, drives up cholesterol levels while also inhibiting the healthy function of insulin. Over time, increased levels of cholesterol in the blood cause the formation of plaques on arterial walls in a process called atherosclerosis. As plaques increase in size, the likelihood of developing heart disease and experiencing a heart attack or stroke increase is immense. The impairment of insulin function increases information and puts you at risk for developing several metabolic conditions such as type 2 diabetes and fatty liver disease.
6. Limit Added Sugars and Refined Grains
Added sugars and refined grains are also significant sources of inflammation in the American diet. Added sugars can be described as sugars that have been removed from their original source and artificially added to packaged foods. When we eat added sugars, the sugar is rapidly broken down into glucose molecules which are then absorbed into the bloodstream. When glucose enters the bloodstream it drives up blood sugar levels significantly. High blood sugar levels have implications for metabolic health.
High levels of blood sugar over time contribute to the risk of insulin resistance, type 2 diabetes, obesity, and fatty liver disease. Moreover, as high levels of glucose course through the blood vessels, the sugar is carried to nearly all body tissues. All organ systems become exposed to unnaturally high levels of glucose. continued exposure to high levels of blood sugar causes inflammation in nearly all body tissues, including the kidneys, the heart, the liver, the joints, and the brain. Eating extra sugar only worsens the pain associated with rheumatoid arthritis.
Refined grains are produced by taking a perfectly healthy grain such as brown rice and removing all nutritional value including protein, fiber, and antioxidants. The remaining product is a starchy, soft grain that is devoid of nutritional value but is more palatable. Refined grains have a nearly identical impact on the body when compared to added sugars. Just like added sugars, refined grains are rapidly broken down into individual glucose molecules, which are then absorbed into the bloodstream to spike blood sugar and cause inflammation.
So, how can you steer clear of added sugars and refined grains in your diet? to avoid added sugars, it’s helpful to know where they might be hiding. Added sugars are sneakily included in more food than you might think. Though added sugars may be an expected ingredient in treats like donuts, cakes, sugary breakfast cereals, pancakes, and pastries, added sugar is also a very common ingredient in foods like bread, ketchup, salad dressings, and granola bars. When trying to avoid added sugars, nutrition labels and ingredients lists are your friends. Keep in mind that certain foods May naturally contain a little bit of sugar and the nutrition label doesn’t necessarily differentiate between the types of sugar. In this case, it’s important to examine the ingredients list for words like “syrup” or anything ending in “-ose.”
To limit the amount of refined grain in your diet avoid foods such as white bread, white rice, cake, cookies, donuts, and pastries.
7. Stick to a Primarily Plant-Based Diet
When it comes to managing rheumatoid arthritis at home, it is critical to stick to a primarily plant-based diet. The diet with the most anti-inflammatory activity is the primarily plant-based Mediterranean diet, which includes an abundance of fruits and vegetables, nuts and seeds, whole grains, beans, and fatty fish rich in omega-3 fatty acids. Keeping your meat and Dairy consumption to a minimum helps reduce the amount of inflammation throughout the body, which is helpful for reducing the frequency of arthritis flare-ups and for quelling the symptoms. Eating too much meat and dairy can increase the levels of trimethylamine oxide in the body, which contributes to systemic inflammation. Eating an abundance of plant-based products and whole foods I’m sure that you’re getting plenty of fiber, vitamins, minerals, and antioxidants in your diet to promote a healthy gut and healthy cellular function.
8. Incorporate Potent Antioxidant and Anti-Inflammatory Foods into Your Diet
In addition to a baseline anti-inflammatory diet, there are specific power foods you can add to your regimen to help soothe rheumatoid arthritis symptoms even more. Green tea contains compounds referred to as EGCG, which is a polyphenol that has long been recognized in Eastern medicine as a healing compound. In more recent research, EGCG has been identified as a helpful compound for reducing inflammation for autoimmune diseases and metabolic conditions like fatty liver disease.
Other Tips
In addition to eating a healthy diet packed with antioxidants, there are some helpful tips that can help you manage rheumatoid arthritis.
Keep a Food Journal
Patients with rheumatoid arthritis often find but they are sensitive to specific foods. However, no two rheumatoid arthritis patients are the same. In order to figure out what foods you may be sensitive to, it’s important to keep a food journal and a daily log of any symptoms you have. Tracking your food intake as well as the pattern of your symptoms can help you pick up on any trends. As a result, you’ll be able to correlate certain foods with your symptoms. if you sent the pattern cut out that screwed and monitor your symptoms.
Lower Stress
Physicians tend to notice that patients report that arthritis flare-ups coincide with periods of increased stress. Physically or emotionally taxing situations tend to elicit a stress response in the body. When the body is undergoing a stress response, this means that cortisol levels epinephrine levels and norepinephrine levels are much higher than usual to help cope with the stressor. If that says stressor is acute and passes in a short. Of time, your levels of stress hormone in the bloodstream will return to normal. However, a chronic physical stressor such as sleep deprivation or chronic emotional stressors such as preparing for a large work presentation may cause chronically elevated levels of stress hormones. Over time, this can lead to systemic inflammation that causes an autoimmune response, leading to joint inflammation.
It’s important to keep stress levels as low as possible. This doesn’t mean to avoid all stressful situations. Stress and stressful circumstances are inevitable parts of life. so we don’t have control over experiencing stress, we do have control over our response to a stressor. Healthy coping mechanisms and stress management techniques can help keep stress hormones low in order to avoid excess inflammation. Yoga, meditation, and deep breathing are helpful techniques for keeping your stress levels at a healthy level.
Exercise Consistently
Exercising is helpful for fighting against obesity, which is a significant risk factor for developing rheumatoid arthritis. Consistently exercising also helps to lower levels of systemic inflammation by promoting the release of anti-inflammatory endorphins.
Conclusion
Rheumatoid arthritis is a common condition that most often affects the joints of fingers and toes. Symptoms of rheumatoid arthritis can extend beyond the joints to affect energy levels and other organ systems such as the kidneys and the eyes. Even though rheumatoid arthritis is a lifelong condition, there are complementary medical interventions and lifestyle interventions that compound one another to promote the best possible outcome. Eating an anti-inflammatory Mediterranean diet filled with fruits, veggies, omega-3 fatty acids, and optimal ratios of amino acids help soothe symptoms and reduce the frequency of flare-ups.
References
(1) https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648