If you have been recently diagnosed with PCOS, then you may be navigating treatment options and strategies for managing your condition and associated symptoms. Being able to identify the cause and influential factors in PCOS is helpful for treating the condition. So, is PCOS genetic or environmental?
The short answer is PCOS develops as a result of both environmental and genetic causes. Read on to find out more about hereditary factors that influence PCOS, as well as environmental factors.
What to Know About PCOS
Before we dive into the genetic and environmental factors influencing PCOS, let’s first talk about what it means to have PCOS.
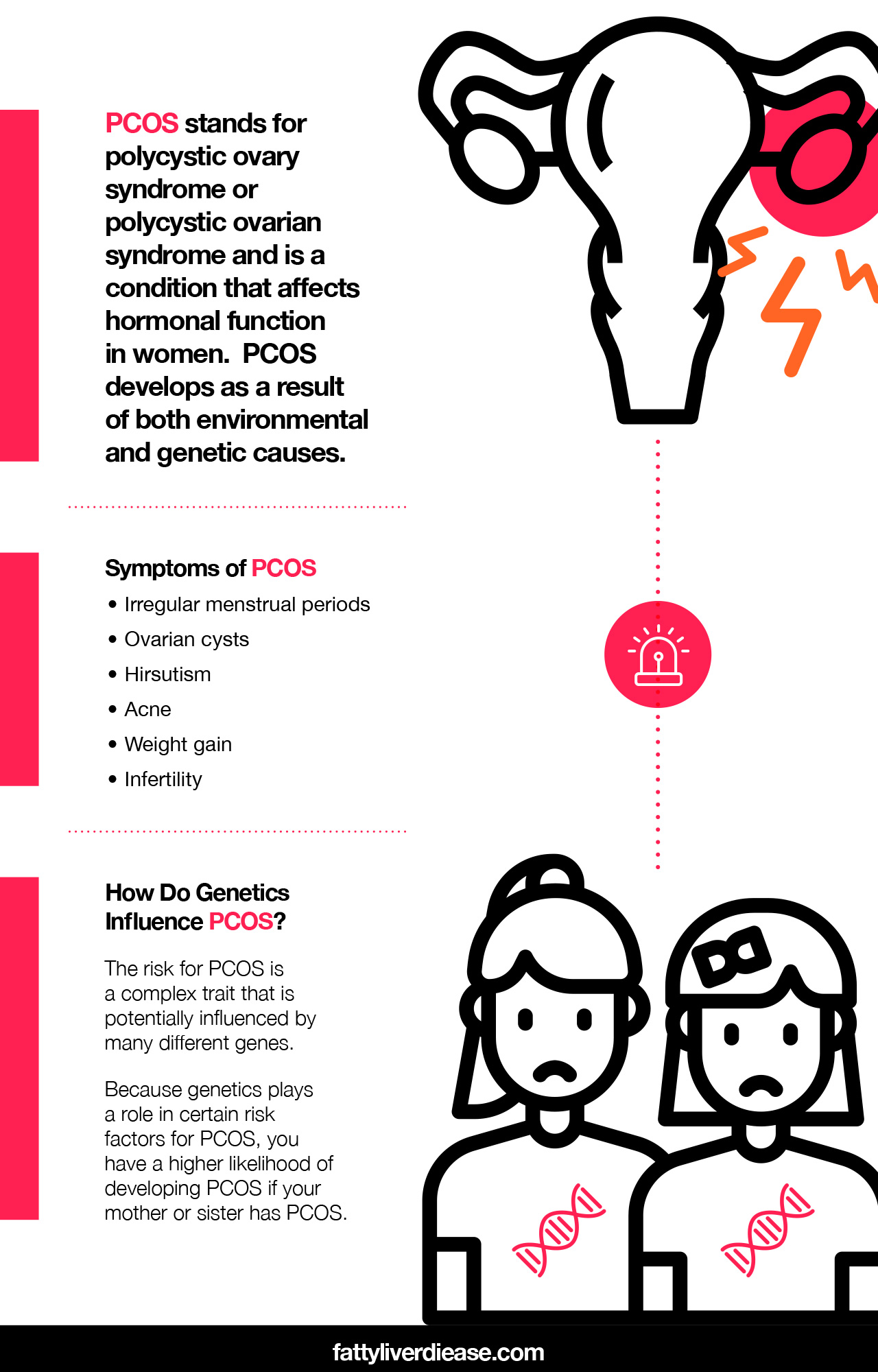
PCOS stands for polycystic ovary syndrome or polycystic ovarian syndrome and is a condition that affects hormonal function in women. PCOS affects the endocrine system, which is responsible for producing hormones, which serve as messengers between organs in the body, to keep all body functions balanced and functioning normally.
In PCOS, reproductive hormones don’t work as they should. Estrogen and progesterone don’t send the right messages to the ovaries and uterus. The body also produces too much testosterone, which is a male hormone. Women with PCOS are prone to having high levels of cortisol, which is a stress hormone. Additionally, PCOS is associated with metabolic dysfunction, and women with the condition are more likely to be overweight and insulin resistant.
Symptoms of PCOS include:
- Irregular menstrual periods: Women with PCOS often experience irregular periods or the absence of a period (amenorrhea). Occasionally, women may also experience PCOS pain. Pain may present as aching in the ovaries or painful periods.
- Ovarian cysts: A PCOS ultrasound may reveal the presence of ovarian cysts, which are fluid-filled pouches or ovarian follicles.
- Hirsutism: Hirsutism is the growth of hair in a male pattern, including on the face and chest.
- Hair loss: Women with PCOS may experience male-pattern baldness on the head.
- Acne: PCOS acne is common. Androgen excess among women with PCOS results in the development of cystic acne on the jawline or lower cheeks.
- Weight gain: Women may experience PCOS weight gain. Weight gain may accompany PCOS because of metabolic disturbances, including insulin resistance and impaired metabolism.
- Infertility: PCOS may result in infertility. Because of hormonal imbalances, and ovarian follicle does not reach maturity and fails to release an egg. The absence of ovulation is referred to as anovulation. As a result, ovulation does not occur, impairing the conception process. However, infertility is not permanent and resolves when symptoms are improved and hormonal imbalances are corrected.
Diagnosis of PCOS
Keep in mind that PCOS must be diagnosed by your physician. Specialists in gynecology and obstetrics and endocrinology often diagnose and treat PCOS. Blood tests, ultrasound exams, and the presence of symptoms play a role in determining a diagnosis.
- Blood tests: Blood tests are valuable tools in the diagnosis of PCOS. Blood tests can reveal biochemical abnormalities in the blood that point towards PCOS. One of the primary indicators of PCOS is excess androgens in the blood. Physicians may also want to gain a better understanding of your endocrine function by testing levels of sex hormone-binding globulin (SHBG), follicle-stimulating hormone (FSH), and luteinizing hormone.
- Ultrasounds: A PCOS ultrasound may reveal ovarian follicle abnormalities. Women with PCOS may have a higher number of follicles than normal. Ovarian enlargement may also be observed, as well as a thicker endometrial lining.
- Evaluating symptoms: Physicians will evaluate your symptoms for signs of hyperandrogenism, like abnormal hair growth patterns and acne. Your doctor will also look for reported irregularities with your menstrual cycles.
- Eliminate other possible causes: Adrenal hyperplasia, thyroid conditions, pregnancy, and hyperprolactinemia may cause many of the same symptoms as PCOS. Adrenal hyperplasia and thyroid conditions may cause excess androgen secretion. The lack of a menstrual cycle during pregnancy may also be confused with PCOS. Your doctor will likely conduct tests to rule out these conditions. For example, a blood test for human chorionic gonadotropin (hCG) can help determine pregnancy.
- Co-occurring metabolic conditions: It is extremely common for women with PCOS to also have conditions associated with metabolic syndrome. Your physician may screen for type 2 diabetes, insulin resistance, high insulin levels or hyperinsulinemia, high blood glucose,
How Do Genetics Influence PCOS?
First, to understand how PCOS can be hereditary, it helps to understand how genes work. Every characteristic and physiological function is determined by a set of instructions written into our DNA. In scientific terms, the characteristic or trait is called the phenotype, and the DNA coding is called the genotype.
Strands of DNA are organized into chromosomes, which are organized into homologous pairs. In each chromosome, you have two copies of each gene – one that you inherited from mom, and one that you inherited from dad. Some traits, such as eye color are controlled by one gene location. Other traits, such as the risk for cardiovascular disease, are influenced by numerous gene locations.
The etiology of PCOS is in part influenced by genetics. The risk for PCOS is a complex trait that is potentially influenced by many different genes. Research published in The Application of Clinical Genetics determines that there is a genetic basis of PCOS and numerous polymorphisms that may influence the development of PCOS. (1)
A candidate gene is one that is a suspect for causing a certain condition, based on its location on the chromosome. Potential candidate genes for PCOS may be those that are influencing insulin function. Research suggests that areas of DNA close to the insulin receptor gene may play a particularly important role in determining the risk of developing PCOS. However, there is not one single gene that predicts whether an individual will develop PCOS or not. Rather, numerous genes play a role in influencing hormonal and metabolic processes.
Genome-wide association studies also help determine if any particular gene is associated with a condition, like PCOS. (2)
A meta-analysis published in PLoS Genetics reports several gene loci or locations that are implicated in the development of PCOS. (3) The analysis determined genes that play a role in both the development of PCOS and metabolic syndrome. (3)
Additionally, a study published in Endocrine Reviews and conducted by Diamanti-Kandarakis et al describes the genetics and phenotypes of PCOS and insulin resistance. (4) The study also asserts that genetic risk is similar across Asian and Caucasian women. (4)
Because genetics plays a role in certain risk factors for PCOS, you have a higher likelihood of developing PCOS if your mother or sister has PCOS.
How Does the Environment Affect PCOS?
Although certain genetic factors may influence the risk for developing PCOS, having a genetic susceptibility does not mean you will definitely develop PCOS. It also doesn’t mean that PCOS is a permanent condition. Environmental factors interact with your DNA, activating certain genes while silencing others from expression. These environmental influences cause a chemical change to DNA called methylation, which impacts how the DNA is expressed. The impact of environmental factors on genetic expression is called epigenetics.
Certain diet and lifestyle choices may influence your genes and may impact metabolic and hormonal function, making it more likely to develop PCOS. At the same time, a healthy diet and lifestyle promotes good metabolic and hormonal function and can reverse the symptoms of PCOS.
Environmental Changes to Reverse PCOS
Certain dietary and lifestyle factors may play a role in the pathogenesis of PCOS. There are several changes you can make to your diet and lifestyle that essentially override what your genetics say. Here are a few steps you can take to reverse PCOS and promote healthy metabolic functioning.
1. Avoid Sugar and Saturated Fat
Avoiding sugar and saturated fat in your diet is an important strategy for reversing PCOS symptoms while also encouraging healthy metabolic function. Both added sugars and saturated fat are present in abundance on the typical American diet.
So, what exactly is the impact of added sugars and saturated fat, when it comes to metabolic and hormonal function? Saturated fat and sugar work together in the body to disrupt normal metabolic and hormonal functioning.
Added Sugars
First, let’s talk about the role of excess sugar in the body. When we eat lots of sugary foods and refined carbohydrates, glucose rapidly enters the bloodstream and raises blood sugar levels. As a result of high blood sugar levels, the body responds by releasing lots of insulin, which is a hormone that signals to cells and organs to utilize sugar from the bloodstream as energy. However, when blood sugar levels are too high, the body can’t handle all of the sugar efficiently. Insulin becomes desensitized to blood sugar. As a result, the sugars are converted to fat and stored throughout the body.
This is the reason why over time, excess sugar consumption increases the risk of fatty liver disease, obesity, type 2 diabetes, and insulin resistance. You can decrease the sugar content of your diet by cutting out foods like soda, candy, ice cream, pastries, white rice, white pasta, and white bread. Removing added sugars from your diet can improve glucose tolerance and insulin resistance.
Saturated Fat
Eating too much-saturated fat also impacts insulin function in the body. Saturated fat comes from animal products like fatty meat, cheese, milk, butter, and cream. A diet that is chronically high in saturated fat interferes with the metabolism of sugar. Saturated fat particles essentially clog up insulin receptors that are present on cells and tissues throughout the body. As a result, cells receive fewer signals to utilize blood glucose, leading to high blood sugar levels. When paired with a high-sugar diet, eating too much-saturated fat can seriously disrupt metabolic function over time.
Additionally, saturated fat consumption can contribute to high cholesterol, high lipids in the blood, and an increased risk of cardiovascular disease.
Avoiding these foods in your diet helps to increase insulin sensitivity, encourage weight loss, and lower inflammation.
2. Consume a Diet Rich in Protein and Fiber
A diet rich in protein and fiber has a potent anti-inflammatory effect on the body and helps improve metabolic function and hormonal balance. First, both protein and fiber help regulate digestion and allow for the slow, steady release of sugar into the bloodstream. Increasing your intake of protein and fiber-rich foods can be a helpful strategy for preventing high blood sugar and improving insulin resistance.
Protein
Protein is vital in the human diet because it offers amino acids, which are the smallest unit of protein. In particular, essential amino acids are nutritionally required on a daily basis in order to support optimal health. Essential amino acids are the raw materials for producing hormones, neurotransmitters, enzymes, and muscle tissue. Getting optimal ratios of essential amino acids on a daily basis is crucial for supporting ideal metabolic function.
An Italian pilot clinical study found that women with PCOS benefitted from essential amino acid supplementation. (5) Results revealed lower insulin levels, lower levels of testosterone, and improvements in hirsutism. (5)
How can you ensure that you are getting optimal ratios of essential amino acids in your diet? Animal proteins contain ideal ratios of essential amino acids. Choose low-fat animal proteins like chicken breast, low-fat cheese, nonfat Greek yogurt, and skim milk. Fish is also an excellent source of protein that also offers healthy fats.
When following a vegan or plant-based diet, it’s especially important to monitor your protein intake to ensure that you’re getting optimal ratios of essential amino acids. Unlike animal proteins, no single vegetable protein offers all of the essential amino acids that you need. Instead, it’s critical to combine proteins throughout the day, including foods like whole grains, beans, nuts, seeds, and tofu.
Supplementation with essential amino acids is also a great option, to ensure that you’re getting amino acids in optimal ratios. Always make sure to use a high-quality supplement and discuss new supplements with your physician.
Fiber
Dietary fiber significantly improves gut health, which has positive impacts on the rest of the body. When we eat dietary fiber, healthy bacteria in the gut feed on the fiber and produce anti-inflammatory compounds. These compounds are then absorbed into the bloodstream, where they can travel throughout the body and reduce inflammation in other organ systems.
Increasing dietary fiber may have specific implications for women with PCOS. A cohort study published in Food & Nutrition found that PCOS was associated with a low consumption of dietary fiber. (6) Researchers suggested that increased dietary fiber may play an important role in mitigating high androgen levels and insulin resistance among women with PCOS. (6)
3. Replace Bad Fats with Good Fats
Instead of eating a diet rich in saturated fats, replace these unhealthy fats with good fats like polyunsaturated and monounsaturated fats. These healthy fats help reduce inflammation, support healthy cellular function, and provide sustained energy.
In particular, omega-3 fatty acids are a type of polyunsaturated fat that is particularly beneficial for reversing PCOS. Omega-3 fatty acids have potent anti-inflammatory properties and may help improve insulin resistance and other metabolic abnormalities associated with PCOS. The most abundant source of omega-3 fatty acids in the form of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) is fatty fish, like salmon, mackerel, and sardines. Additional supplements may also be beneficial. Certain nuts and seeds like chia seeds, flaxseeds, walnuts, and pecans contain alpha-linolenic acid (ALA), which is the plant form of omega-3 fatty acids.
In general, you can increase the healthy fat content of your diet by eating foods like fatty fish, nuts, seeds, and avocados.
4. Maintain a Healthy Weight
Staying within a healthy body mass index (BMI) range for your height and age is important for balancing your hormones and improving PCOS symptoms. Obese women are at a higher risk of experiencing metabolic abnormalities and hormonal imbalances. In fact, many women experience an improvement of symptoms just with weight loss alone.
If you are overweight and have been diagnosed with PCOS, shedding excess weight and striving for healthy body composition are key steps in managing hormonal imbalances and reversing PCOS. Losing excess body fat can help lower systemic inflammation, supporting a healthy metabolism and balanced hormone levels.
So, how can you encourage fat loss? Eating anti-inflammatory foods, monitoring your caloric intake, and exercising regularly are crucial strategies in helping clear fat deposits from the body. Avoid crash dieting and starvation, which can disrupt metabolic function, worsen blood sugar spikes, and ultimately be counterproductive in managing PCOS.
Talk to Your Doctor About Treatment Options
Medications work with your diet and lifestyle changes to help balance your hormones, manage symptoms, and improve associated metabolic issues. Physicians may prescribe medications to help manage hormonal abnormalities and associated symptoms. Birth control can help regulate your periods, while spironolactone can help treat hyperandrogenemia. Metformin may be prescribed to treat diabetes mellitus and insulin resistance and can play a regulatory role in metabolic function.
Always discuss your lifestyle changes, diet, supplements, and medications with your doctor so you can establish the best treatment plan for your specific needs.
Conclusion: Is PCOS Genetic or Environmental?
PCOS has a high prevalence among American women of reproductive age, and it is influenced by both genetic and environmental factors. Having genetic susceptibility for developing PCOS does not mean that you will definitely get PCOS or that you will have PCOS for the rest of your life. Instead, making changes in your environment can influence how your genes are expressed and effectively reverse PCOS and associated symptoms. Following a few diet and lifestyle changes can make a profound difference in balancing hormones and improving symptoms of PCOS. Keep in mind that it’s always important to talk to your doctor about your diet changes, supplements, and treatment plan to ensure that you’re supporting your health in every way.
References:
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935309/
(2) https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-3492-z
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6300389/
(4) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5393155/























