“Hepatosteatosis” sounds like a long and complicated word, and it can be frightening to receive a diagnosis of hepatosteatosis. Hepatosteatosis is a liver condition that has a high incidence across the American population. What even is hepatosteatosis, and what does it mean for your health? Read on to find out what it means to have hepatosteatosis and what you can do to manage it.
What Is Hepatosteatosis?
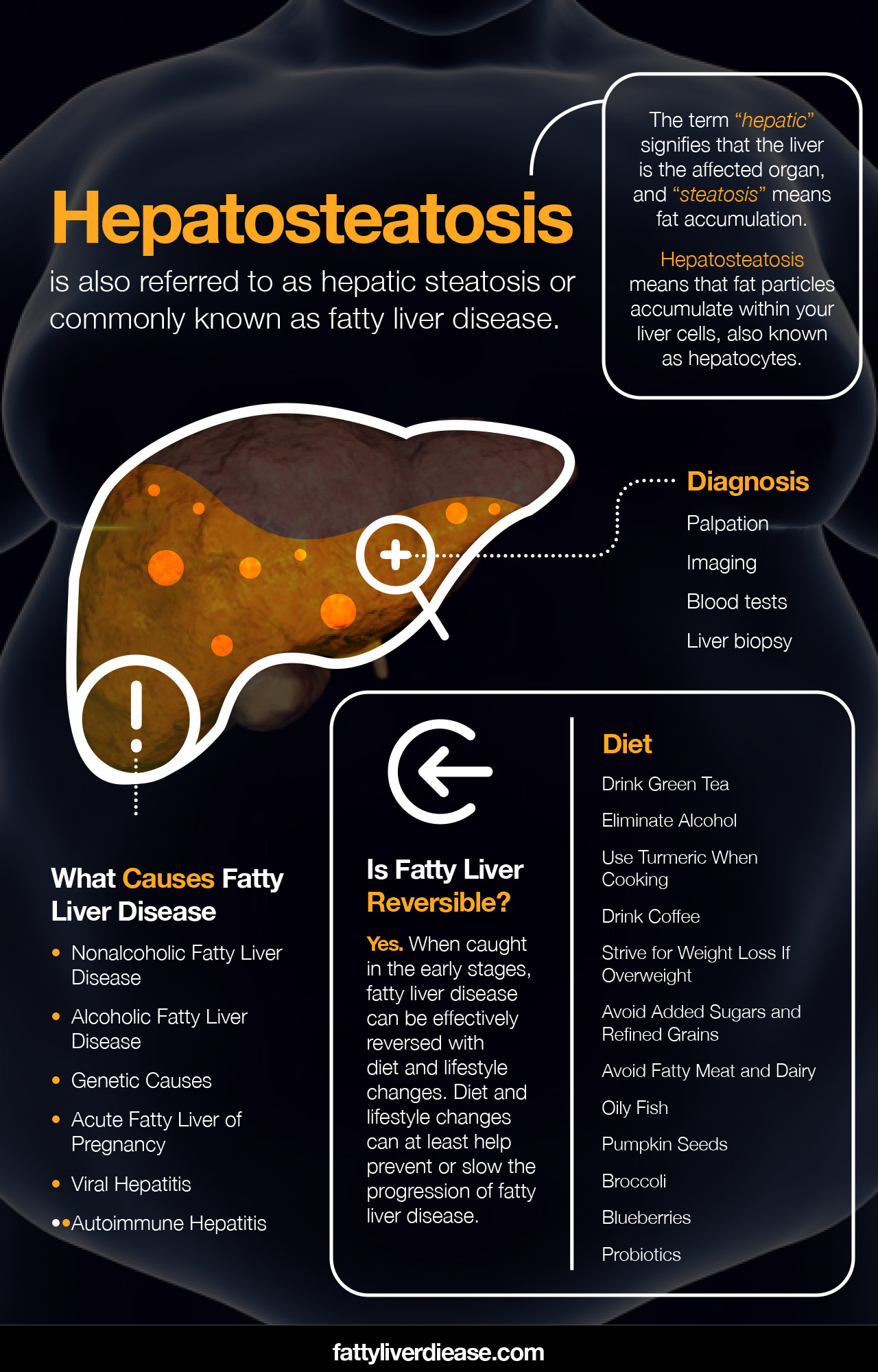
Hepatosteatosis is also referred to as hepatic steatosis or liver steatosis. Most commonly, it is referred to as fatty liver disease. The term “hepatic” signifies that the liver is the affected organ, and “steatosis” means fat accumulation.
As a result, hepatosteatosis means that fat particles accumulate within your liver cells, also known as hepatocytes.
How Are You Diagnosed?
Your doctor may use many diagnostic methods to detect the presence of fatty liver disease.
- Palpation: Your doctor may be able to assess liver inflammation during a physical examination using a method called palpation. If you have fatty liver disease, the combination of inflammation and extra fat cells may cause liver enlargement. Your physician may be able to feel liver enlargement.
- Imaging: Ultrasound technology, magnetic resonance imaging (MRI), and computed tomography (CT) scans may show the echogenicity, shape, and texture of the liver. Imaging can also assess the pattern of hepatic lipid distribution. For example, diffuse hepatic steatosis describes the broader distribution of fat accumulation throughout the liver.
- Blood tests: A blood test can detect your levels of liver enzymes. Elevated liver enzymes like alanine aminotransferase (ALT) and aspartate transaminase (AST) signify liver inflammation and may indicate fatty liver disease.
- Liver biopsy: A liver biopsy is one of the more specific ways to evaluate liver health. A liver biopsy involves taking a tiny liver tissue sample and evaluating it for inflammation, fat accumulation, lesions, or other abnormalities.
What Causes Fatty Liver Disease and Are You at Risk?
Fatty liver disease has several contributing factors. Different individuals experience fat accumulation in the liver for a variety of reasons.
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease – also referred to as NAFLD – has a high prevalence rate among American adults. Nonalcoholic fatty liver disease develops primarily as a result of a poor diet and metabolic dysfunction. Individuals with metabolic syndrome tend to be at an increased risk of developing fatty liver disease.
Insulin resistance, obesity, type 2 diabetes, and high triglycerides are all risk factors that correlate with a higher likelihood of developing fatty liver disease. Cardiovascular issues may also be connected to fatty liver disease and metabolic syndrome.
Alcoholic Fatty Liver Disease
Alcoholic fatty liver disease – also referred to as AFLD – is caused by the chronic consumption of excess alcohol and therefore has different pathogenesis than nonalcoholic fatty liver disease. Alcohol is essentially a toxin and must be detoxified by the liver. Chronic alcohol consumption causes the accumulation of free radicals in liver cells, resulting in oxidative damage in liver tissues. Alcohol consumption leads to the development of alcoholic fatty liver disease.
Genetic Causes
Some individuals may be genetically prone to developing fatty liver disease. Certain genetic disorders, such as hemochromatosis and Wilson’s disease, cause abnormal metabolic processes in the liver. Over time, these genetic conditions may cause inflammation and scarring.
Though the exact genes haven’t been identified, it seems that there is a genetic component to developing fatty liver disease. Having a family history of fatty liver disease tends to be one of the predictors for developing the condition.
Acute Fatty Liver of Pregnancy
Though rare, fatty liver disease may develop spontaneously during pregnancy. Women are more at risk for developing acute fatty liver of pregnancy when their baby has unusual lipid metabolism processes.
Viral Hepatitis
Hepatitis A, hepatitis B, and hepatitis C may contribute to the development of fatty liver disease over time. Hepatitis A and B are less common in the United States, and the hepatitis C virus is the most commonly associated with liver cirrhosis.
Autoimmune Hepatitis
Unlike viral hepatitis, autoimmune hepatitis does not develop as a result of a viral infection. Instead, autoimmune hepatitis develops as a result of the over-activation of the immune system. Autoimmune hepatitis is caused by a malfunctioning immune system that attacks healthy liver tissue and causes damage.
Does Hepatosteatosis Progress?
Unfortunately, hepatosteatosis may progress to more severe forms of liver disease. Fatty liver disease, over many years, may progress to nonalcoholic steatohepatitis (NASH). Steatohepatitis describes a chronic state of inflammation in the liver. In an inflamed state, liver cells function more slowly and cannot carry out their job effectively.
Over time, chronic steatohepatitis may result in the production of scar tissue through a process called fibrosis. Liver fibrosis may ultimately cause liver cirrhosis. Chronic liver disease causes constant damage to the liver, which can also increase the risk of developing hepatocellular carcinoma, or liver cancer.
The good news is that if you begin treatment early, you can decrease the chances of your liver condition progressing to more severe conditions. Keep reading to find out how you can reverse fatty liver disease and help prevent progression.
Is Fatty Liver Reversible? What You Can Do to Manage Fatty Liver Disease
Can fatty liver be reversed? Yes. The good news is that fatty liver disease is reversible. When caught in the early stages, fatty liver disease can be effectively reversed with diet and lifestyle changes. When caught in later stages such as steatohepatitis and fibrosis, fatty liver disease may still be reversible, though not completely. Diet and lifestyle changes can at least help prevent or slow the progression of fatty liver disease.
1. Drink Green Tea
In Chinese medicine, green tea has been considered a therapeutic herb for many centuries. Did you know that green tea may help reverse fatty liver disease? In fact, a review published in Nutrition Reviews found that green tea may have liver-protecting properties that help reverse fatty liver disease. (1) In particular, the polyphenols found in green tea have potent antioxidant activity and help reduce inflammation and lipid accumulation in the liver.
So, how can you incorporate green tea into your daily routine? Try drinking a cup of green tea in the mornings, in addition to your coffee. Because green tea contains both antioxidants and caffeine, it can have an energizing effect. It may be best to consume green tea in the mornings so that it doesn’t disturb your sleep.
If you were not wild about the taste of green tea, you can brew it and add it to green juices or smoothies of your choice. The taste of green tea is mild enough that it is easily drowned out by other flavors such as fruit or chocolate.
2. Eliminate Alcohol
Eliminating alcohol from your diet is a critical step in managing body liver disease. If you continue to drink alcohol, other treatment methods will not be as effective. First and foremost, it’s essential to eliminate alcohol intake so that your body can effectively work on healing.
If you are physically dependent on alcohol, it is critical to establish a plan to wean yourself off alcohol and become sober. The detox process for alcoholism is tough and is accompanied by many unpleasant symptoms such as shaking, sweating, vomiting, and a rapid heart rate. In severe cases, detoxing from alcohol may cause delirium tremens, which results in serious symptoms like hallucinations and seizures. If you plan to detox from alcohol, it’s important to first seek medical advice and come up with a safe plan.
3. Use Turmeric When Cooking
Turmeric- also known as curcumin – is a spice often used in Eastern cooking. In Eastern medicine, turmeric has long been recognized for its therapeutic properties. Research shows the many healing properties of turmeric, including the potential for improving fatty liver disease. A systematic review published in Integrated Medicine Research found that turmeric supplementation is associated with an improvement in liver enzyme levels for individuals with fatty liver disease. (2)
Try adding turmeric to savory dishes like curry, chili, lentil stew, or soup. Turmeric is subtle in flavor but adds a pleasant warmth to any dish. If you don’t enjoy the flavor of turmeric, you can easily disguise it in fruit-based smoothies or juices. Alternatively, you can prepare a “turmeric shot” by mixing it into the water and quickly drinking it. When possible, try to add both turmeric and black pepper to your food. Black pepper facilitates the absorption of turmeric significantly.
If you opt for a turmeric supplement, always talk to your doctor before adding supplements to your regimen.
4. Drink Coffee
We may love coffee because it helps us wake up in the mornings or stay up later when needed, but did you know that drinking coffee has hepatoprotective effects? Drinking coffee is associated with lower levels of liver enzymes and may also have anti-fibrotic properties.
Regularly drinking coffee may help prevent fatty liver disease from progressing. To reap the liver benefits that coffee has to offer, aim to drink 1-2 cups of regular brewed coffee each day. Avoid adding excess sugar and cream, and stick to low-calorie, low-fat, and low-sugar options like almond milk and skim milk.
5. Strive for Weight Loss If Overweight
Being overweight or obese significantly increases the risk of developing fatty liver disease. When carrying excess fat, the body accumulates adipose tissue in areas like the legs, abdomen, and arms. The liver
Moreover, being overweight increases the likelihood of experiencing metabolic dysfunction. Excess fat tissue contributes to systemic inflammation and maladaptive mechanisms for processing sugar. When overweight, fat tends to accumulate in the liver more easily.
To lose weight, it’s vital to eat the number of calories that supports your ideal body weight. Make sure that the number of calories you consume is carefully planned to take into account your metabolism and activity levels. A registered dietitian or nutritionist is a valuable resource in planning a weight loss regimen that is tailored to suit your needs.
One word of caution, however; avoid losing weight too rapidly. Severe caloric restriction and subsequent malnutrition may rarely precipitate fatty liver disease and steatohepatitis. (3)
6. Avoid Added Sugars and Refined Grains
The chronic consumption of added sugars and refined grains is a major contributor to the development of the fatty liver disease. The body handles the simple carbohydrates and added sugars and refined grains using the same mechanism. For example, when we eat a pastry packed with refined sugar and grains, the body rapidly breaks down these ingredients into glucose molecules. Glucose is quickly absorbed into the bloodstream and spikes blood sugar.
In response to high blood sugar levels, the pancreas releases a hormone called insulin. Insulin is responsible for indicating to body cells that they should utilize glucose for energy. However, insulin and cells are generally no match for chronic bursts of blood sugar, and excess sugar is inevitably deposited throughout the body as fat.
You can avoid consuming too much-added sugars and refined grains by steering clear of soda, candy, pastries, sugary breakfast cereals, white bread, white rice, and white pasta. When purchasing packaged food items, it’s a good idea to assess the nutrition label and ingredients list to ensure that there are no added sugars. You might be surprised how much sugar is added to seemingly benign items like salad dressings and yogurt.
7. Avoid Fatty Meat and Dairy
Fatty meat and dairy products are unhealthy for fatty liver disease because they exacerbate inflammation and contribute to metabolic dysfunction. Fatty meat and dairy contain high levels of saturated fat. Moreover, saturated fat is known to increase cholesterol levels and lead to plaque buildup in the arteries through a process known as atherosclerosis. Over time, excess saturated fat consumption can lead to the accumulation of plaques and subsequent increased risk of having a heart attack or developing heart disease.
Moreover, saturated fat can also clog up insulin receptors, making it difficult for insulin to function as it should. This, in turn, can lead to further metabolic issues, chronically high blood sugar, and increased fat deposits in the liver.
8. Oily Fish
Unlike fatty meat and dairy products, oily fish is packed with healthy polyunsaturated fats in the form of omega-3 fatty acids. The type of omega-3 fatty acids found in fish includes eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Both forms of omega-3 fatty acids reduce inflammation throughout the body, helping to improve liver health.
To increase your intake of EPA and DHA, consume several servings of fatty fish per week. Healthy options include salmon, mackerel, and sardines. Keep in mind that during pregnancy, fish consumption should be kept to a minimum and certain fish should be avoided. Always consult your physician or a registered dietitian for advice regarding your diet and your specific health needs.
9. Pumpkin Seeds
Research shows that pumpkin seed oil has beneficial effects on inflammation and nonalcoholic fatty liver disease. (4) Researchers have also found that virgin pumpkin seed oil had a more positive impact than processed oil. (4)
Pumpkin seeds and pumpkin seed oil are rich in polyunsaturated fats and phytochemicals that fight against inflammation. Replacing unhealthy fats in your diet with polyunsaturated fats from plant sources can help decrease oxidative stress and inflammation in the liver. Whole pumpkin seeds are also a healthy source of polyunsaturated fats and antioxidants. Walnuts, pecans, flaxseeds, and chia seeds are also excellent sources of polyunsaturated fats.
10. Broccoli
As kids, we might’ve been told to eat our broccoli because it helped us grow big and strong. But did you also know that broccoli can help fight against fatty liver disease? A study published in the Journal of Functional Foods assessed the impact of broccoli feeding on mice who were exposed to a chemical known to be toxic to the liver. (5) Results found that consuming broccoli protected the livers from lipid accumulation though not from liver cancer. (5)
Sulforaphane is thought to be the component in broccoli that exhibits hepatoprotective properties. Other foods with sulforaphane include kale, cauliflower, cabbage, and mustard greens.
In addition to sulforaphane, fruits and veggies contain a variety of antioxidants that may be beneficial for fatty liver disease. Brightly colored fruits and vegetables signify the presence of lots of antioxidants like polyphenols and carotenoids. Different colors also represent different antioxidant content. Eating a variety of different colors in your fresh produce will ensure that you’re getting many different kinds of antioxidants, like flavonoids, flavanols, beta carotene, and lycopene. For example, strawberries, blueberries, persimmons, oranges, watermelon, papaya, spinach, Brussels sprouts, and sweet potatoes are excellent foods to incorporate into your diet.
11. Blueberries
Research has shown that the combination of blueberries and probiotics seems to attenuate fatty liver disease. (6)
Blueberries are rich in polyphenols and other micronutrients that can help lower inflammation and oxidative stress associated with fatty liver disease. Try sprinkling blueberries in your oatmeal, on your oatmeal, or simply eating them by the handful. Blueberries are also a delicious component on fruit salads or a sweet component on green salads.
12. Probiotics
Probiotics have been shown to have a therapeutic effect on nonalcoholic fatty liver disease. A meta-analysis published in Therapeutic Advances in Gastroenterology demonstrates that studies reveal a link between probiotics and lower levels of liver enzymes, improves cholesterol levels, lower levels of inflammation, and lower blood glucose levels. (7)
What are probiotics, anyway? Probiotics are healthy bacteria that help break down the food that you eat.
Probiotics can be found in a variety of foods. Sauerkraut, low-fat yogurt, kefir, kombucha, and kimchi are rich in healthy bacteria for the gut.
Eating foods rich in fiber also supports a healthy gut microbiome. Fiber feeds healthy bacteria in the gut. In turn, these good bacteria produce anti-inflammatory compounds that are absorbed through the small intestine and into the bloodstream. These compounds can produce an anti-inflammatory effect in many areas of the body, including the liver.
Things to Keep in Mind
If you are concerned about your liver function or possible liver damage, it’s important to make an appointment with your doctor. Your primary care physician can conduct necessary tests and refer you to specialists in hepatology and gastroenterology to ensure that you get an accurate diagnosis and timely treatment plan.
Hepatosteatosis: Conclusion
Hepatosteatosis is a condition that describes the buildup of fat in liver cells. Hepatosteatosis may accompany conditions like nonalcoholic fatty liver disease and alcoholic fatty liver disease. When diagnosed in earlier stages, fatty liver disease can be reversed with diet and lifestyle changes. Eating lots of healthy fats, high-quality protein, fruits and veggies, and fiber is critical for reversing fatty liver disease. It’s also important to avoid added sugar, refined grains, alcohol, and saturated fat to promote liver health.
References:
(1) https://pubmed.ncbi.nlm.nih.gov/22221215/
(2) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6428926/
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5935795/
(4) https://pubmed.ncbi.nlm.nih.gov/26405765/
(5) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5034860/























