So, you’ve been diagnosed with hepatic encephalopathy. Receiving a diagnosis like hepatic encephalopathy can be scary and may leave you feeling uncertain about what to do next. Luckily, there are actions you can take in your daily life to help reverse your symptoms and take care of your liver and brain.
Hepatic encephalopathy describes the cognitive and neurological symptoms resulting specifically from liver disease. Here we discuss the biological basis of your condition and how nutrition can support healing. Understanding your diagnosis will empower you to take proactive steps to manage your symptoms and increase your quality of life.
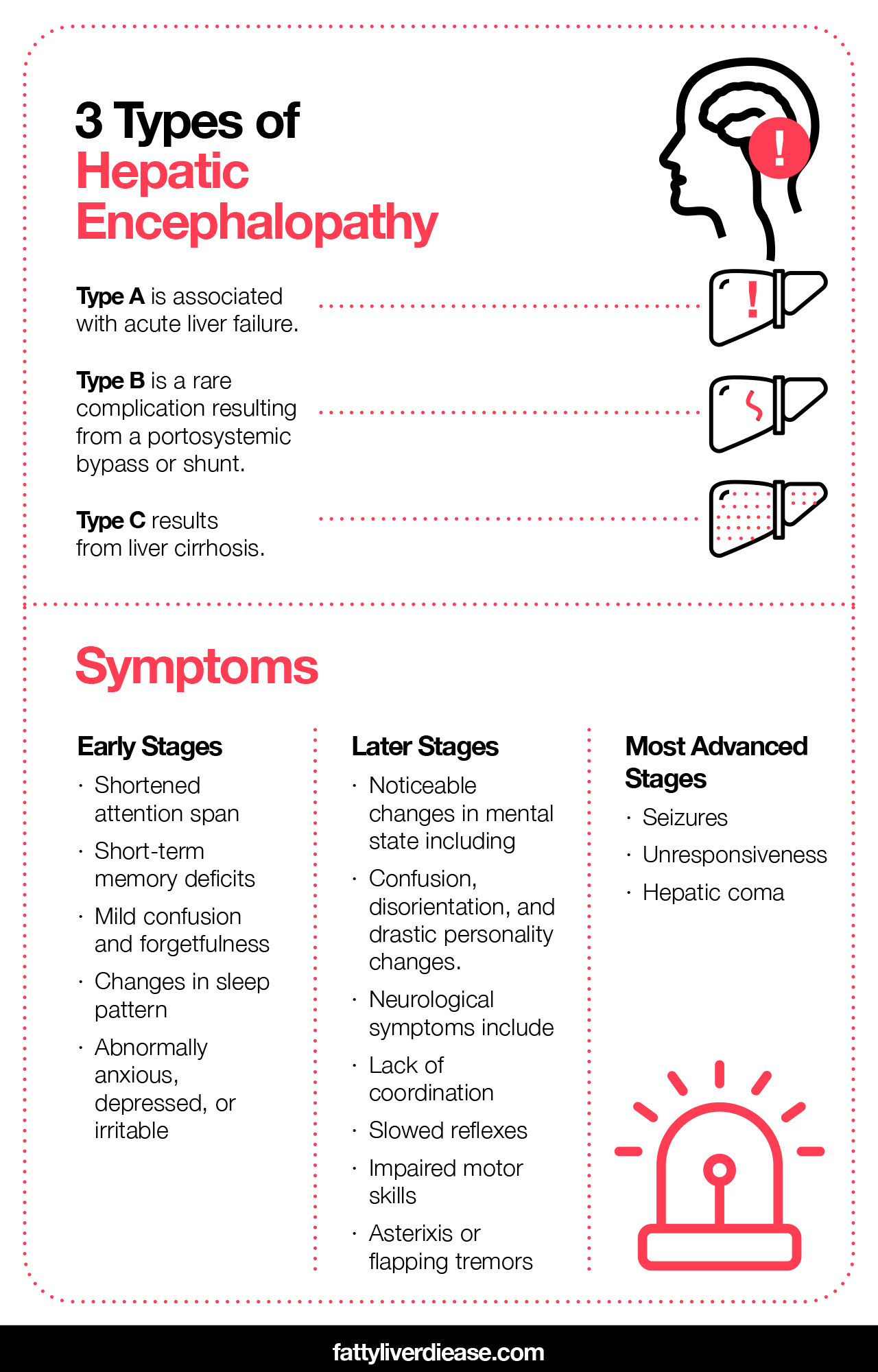
3 Types of Hepatic Encephalopathy
Let’s first take a look at the types of hepatic encephalopathy and the symptoms you may be experiencing. Types of hepatic encephalopathy are sorted according to the origin of liver damage.
- Type A is associated with acute liver failure. Acute liver failure is the sudden and rapid deterioration of liver function and can be brought on by drug toxicity, like excessive intake of acetaminophen (the compound found in Tylenol). Other causes include viral infections like hepatitis.
- Type B is not related to an underlying disease. This type of hepatic encephalopathy is instead a rare complication resulting from a portosystemic bypass or shunt. Portosystemic shunting can be either a congenital defect or a surgically placed treatment for high blood pressure in the portal vein, a condition called portal hypertension.
- Type C results from liver cirrhosis. Cirrhosis refers to scarring of the liver tissue. When structurally damaged, normally functioning soft liver tissue turns into dense scar tissue.
Most cases of hepatic encephalopathy are associated with liver cirrhosis. Cirrhosis is commonly caused by alcoholism, hepatitis C and B, and non-alcoholic fatty liver disease. It is estimated that the vast majority – nearly 80% – of individuals with cirrhosis will experience symptoms of hepatic encephalopathy.
Severity of Symptoms Exists on a Spectrum
If you’ve been diagnosed with hepatic encephalopathy, you may be experiencing a range of symptoms impacting your cognitive function. Some symptoms are so subtle that you may hardly notice them; others are extreme.
Early Stages
The early stages of the disease are referred to as minimal hepatic encephalopathy. Though the results of neurological exams are normal, you may experience a shortened attention span, short-term memory deficits, mild confusion, and forgetfulness. You may notice changes in your sleep pattern and feel abnormally anxious, depressed, or irritable. These symptoms can sometimes be mistakenly attributed to psychiatric illnesses or other brain disorders.
Later Stages
Progressing through the hepatic encephalopathy stages, your cognitive functioning becomes increasingly impaired, and symptoms may become disruptive to your daily life. Noticeable changes occur in your mental status, including confusion, disorientation, and drastic personality changes. Neurological symptoms include lack of coordination, slowed reflexes, and impaired motor skills. Asterixis, or flapping tremors, is also commonly observed. The most advanced stages are characterized by seizures, unresponsiveness, and hepatic coma.
Prognosis
The hepatic encephalopathy life expectancy varies and ultimately depends upon the type and severity of the liver disease. For example, the prognosis for acute liver failure is much worse than that of cirrhosis. Keep in mind that hepatic encephalopathy is generally described as a reversible condition, and there are things you can do to heal liver damage and prevent disease progression.
Biological Interaction Between Your Liver and Your Brain
Before we dive into the curative steps, it’s helpful to understand how your symptoms are a product of all of the events happening in your body on a molecular level. Let’s take a look at how the liver is vital for nearly all physiological mechanisms, and what happens when hepatic processes malfunction.
How the Liver Functions
You can think of the liver as your body’s highly efficient chemistry lab. The liver maintains biochemical homeostasis by regulating blood volume, detoxifying harmful compounds, harnessing energy, and optimizing immune system response. The liver plays a key role in breaking down macronutrients– proteins, carbohydrates, and fats- and synthesizing blood proteins like albumin and clotting factors.
Liver cells contain specialized enzymes, which are proteins that can alter molecular compounds. When food, alcohol, or medications are consumed, macronutrients and toxins pass through the digestive system and are sent to the liver through the portal vein. The liver processes proteins, carbohydrates, and fats for immediate use by the body and converts excess energy into storable forms to be used when needed.
Liver proteins like cytochrome p450 enzymes and transferases are involved in detoxifying compounds. It’s important to note that toxins are not limited to drugs and alcohol- toxins can also refer to pollutants and allergens. Even metabolic byproducts can be toxic, requiring processing by the liver.
Liver Disease Impacts the Brain
Though the liver and brain are located in physically separate areas of the body, the functions of these two organs are intimately connected.
When damaged or diseased, the liver will mistakenly manufacture defective compounds or fail to detoxify harmful substances. So, how does this impact the brain? Toxic compounds are not quarantined in the liver; instead, they accumulate in the bloodstream and are subsequently carried to the brain.
Your brain is protected by the blood-brain barrier, which is selectively penetrable and blocks the entry of many toxic compounds. However, the blood-brain barrier is unable to filter out all toxins. If blood levels of toxins get too high, toxic compounds can cross this protective filter and interfere with healthy neurological functioning.
What Causes Hepatic Encephalopathy Symptoms?
The pathogenesis of hepatic encephalopathy is complex and still under investigation. Researchers in hepatology have identified specific compounds called neurotoxins that lead to impaired brain function and the clinical manifestations of hepatic encephalopathy. Ammonia is one of the most studied neurotoxins implicated in hepatic encephalopathy.
Ammonia is Highly Toxic to Your Brain
Ammonia is a poisonous byproduct of protein breakdown and digestive processes. Healthy liver tissue utilizes the urea cycle to convert ammonia into a non-toxic form. However, the urea cycle is compromised in cirrhotic livers, leading to a buildup of ammonia in the blood – a condition called hyperammonemia.
Ammonia inhibits the expression of genes found in neurons, resulting in deformed brain proteins and impaired communication among neurotransmitters. Ammonia also damages astrocytes- cells involved in immune response in the central nervous system, including the brain. In the presence of ammonia, astrocytes lose their structural integrity, absorb excess water, and cause the brain to swell.
Malnutrition is Connected to Liver Disease and Hepatic Encephalopathy
Individuals with chronic liver disease are particularly prone to being malnourished. The liver is central to breaking down and utilizing nutrients from food. Disruptions in these processes lead to metabolic issues like increased insulin resistance, decreased protein synthesis, and poor absorption of nutrients. Additional symptoms associated with liver disease, like nausea and loss of appetite, reinforce malnutrition due to insufficient food intake.
Malnutrition Makes You Lose Muscle Mass
Across the board, maintaining muscle mass is important for good health, but it’s especially important if you have hepatic encephalopathy. Liver disease makes you particularly prone to loss of skeletal muscle due to metabolic changes and subsequent malnutrition. For comparison, an individual with liver disease reaches a fasting metabolic state overnight; for a healthy individual, it takes three days to reach the same metabolic state. This accelerated fasting state contributes to the rapid loss of both muscle and fat.
You Need Muscle Cells to Detoxify Ammonia
When the liver is damaged and unable to function at full capacity, skeletal muscle takes over as your body’s main processing plant for ammonia detoxification. Skeletal muscle cells use free ammonia from the bloodstream to synthesize an amino acid called glutamine. In the absence of skeletal muscle, ammonia continues to build up in the bloodstream and exacerbate cognitive symptoms.
Medical Interventions for Hepatic Encephalopathy
Management of hepatic encephalopathy often requires medical treatment and is centered around controlling ammonia levels. Studies have shown that antibiotics like rifaximin or neomycin help keep serum ammonia levels low. Administering lactulose also helps control ammonia levels in the blood by decreasing the production of ammonia in the intestines. In other cases, artificial devices that mimic liver activity may be used to filter toxins from the blood. In advanced cases of liver failure, liver transplantation may be the best option.
Hepatic encephalopathy treatment plans are designed to both mitigate cognitive symptoms and address liver damage. Like most diseases and conditions, hepatic encephalopathy is most easily reversed when caught in earlier stages. However, our bodies are equipped with remarkable repairing mechanisms and there are many things you can do to support the healing process at any stage.
Regardless of the treatment you need, nutritional plans can enhance the impact of medicine-based interventions. Formulating a plan of attack on both the nutritional and medical fronts is crucial for optimizing health outcomes.
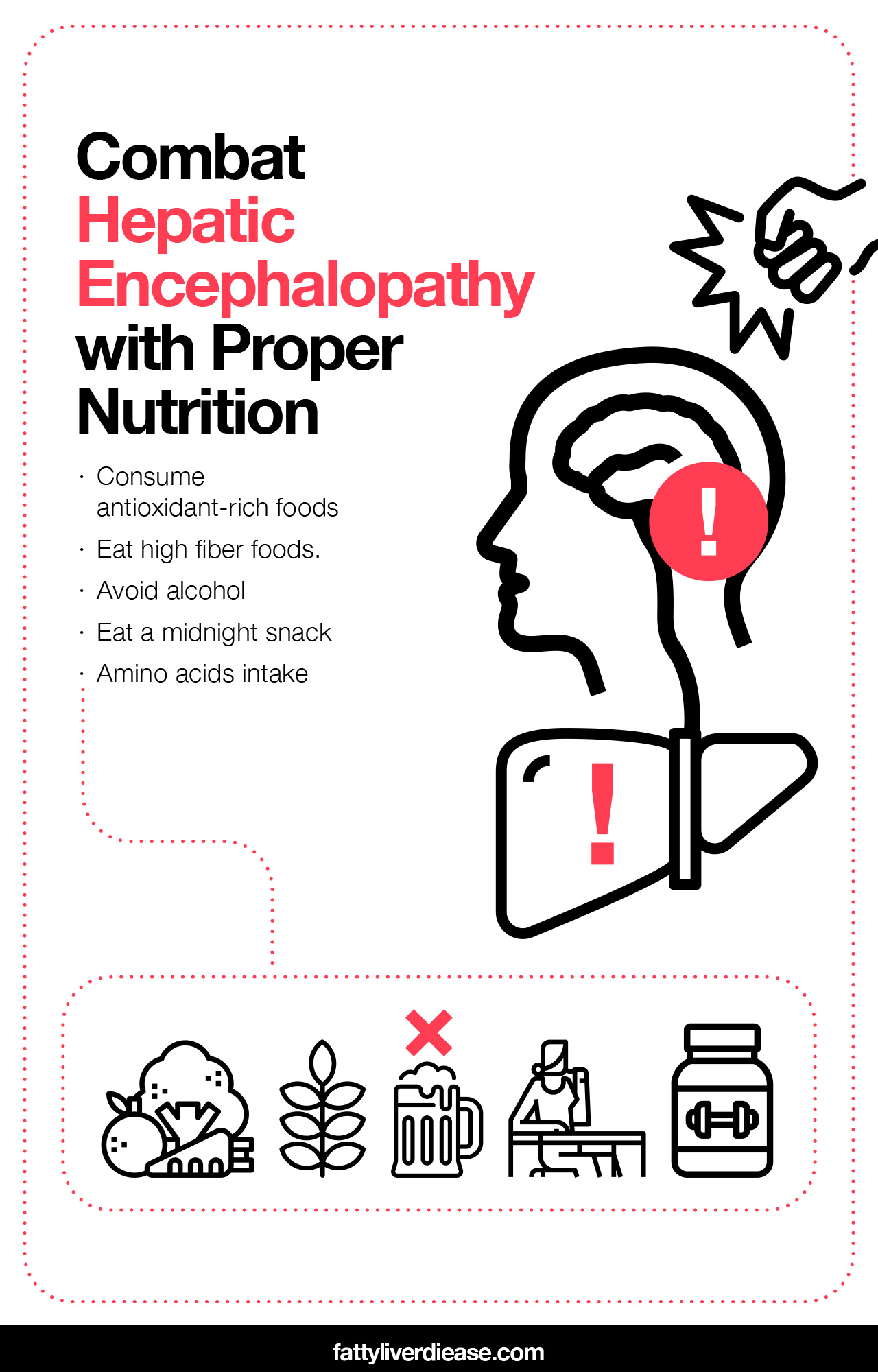
Combat Hepatic Encephalopathy with Proper Nutrition
Counteracting malnutrition is necessary for mitigating symptoms associated with liver failure and hepatic encephalopathy. Additionally, certain biochemical states have been identified as precipitating factors that worsen hepatic encephalopathy in individuals with chronic liver disease.
Below are dietary guidelines you can follow to encourage liver health and manage your symptoms.
- Consume antioxidant-rich foods. Biological processes taking place in the liver produce particles that contain reactive oxygen free radicals. These free radicals interrupt cellular functions, producing a condition called oxidative stress. A diseased liver is particularly vulnerable to damage inflicted by oxidative stress, and consuming foods high in antioxidants can exert protective effects. Research shows that vitamins E, C, and zinc may help protect liver cells from free radical activity. Natural sources of vitamin E include green leafy vegetables and nuts. Vitamin C can be found in peppers, brussels sprouts, and oranges. Zinc can be found in beans, nuts, and seeds.
- Eat high fiber foods. Consuming high fiber foods like fruits, vegetables, and whole grains will expedite the passage of food through the digestive system and create a more acidic digestive environment. This will limit ammonia absorption, therefore controlling blood ammonia levels.
- Avoid alcohol. Alcohol consumption generates a significant amount of oxidative stress in liver cells. Cutting out alcohol will allow the liver to focus on reparative processes, rather than damage control. Alcohol also impacts your immune function by essentially lowering your defenses and making your body more susceptible to viral and bacterial infection. Infections can exacerbate symptoms associated with liver disease because a cirrhotic liver is unable to efficiently modulate the release of biochemicals that play a part in the body’s immune response. As a result, proteins like cytokines may remain activated and contribute to systemic inflammation – a suboptimal condition for healing.
- Eat a midnight snack. Research shows that for individuals with liver cirrhosis, consuming a late-night snack prevents muscle loss. Eating right before bedtime induces healthy metabolic changes that prevent premature fasting.
Another important nutritional suggestion is the consumption of amino acids.
Could Amino Acids Be a Key to Liver Health?
Research explores the particularly important role that amino acids play in liver health and the treatment of hepatic encephalopathy.
What Are Amino Acids?
Amino acids are compounds used in protein synthesis, neurotransmission, and metabolism throughout the body. Amino acids crucial to human biochemistry share the presence of an amine group (a nitrogen atom bonded to two hydrogen atoms) and a carboxyl group (a carbon atom bonded to an oxygen atom and oxygen-hydrogen group).
Amino acids can be categorized as either essential or nonessential amino acids. Nonessential amino acids can be synthesized through our body’s cellular processes; essential amino acids must be consumed through our diet.
Essential Amino Acids and Liver Health: What the Research Shows
Increasing your intake of essential amino acids may help you manage the cognitive symptoms associated with liver disease and may even be a crucial component in reversing liver damage. Research suggests that supplementing with essential amino acids can reduce alcohol-related liver damage. Other studies show that the intake of a balanced formula of essential amino acids may even help prevent liver damage in the first place.
Let’s take a look at some of the essential amino acids to better understand how they positively impact your liver.
Histidine
Histidine plays an important role in immune function and gene expression. In one particular study examining mice, researchers found that histidine protected liver cells from acetaminophen-induced damage by lowering the activity of cytokines. This suggests that consuming foods with histidine may have an anti-inflammatory effect on your liver.
Lysine
Lysine supports immune function and growth and helps harness energy from fat. Research has demonstrated that consuming lysine reverses liver damage inflicted by fatty liver disease – a precursor to liver cirrhosis.
Isoleucine, Leucine, and Valine
Isoleucine, leucine, and valine are referred to as branched-chain amino acids (BCAAs). BCAAs are involved in numerous physiological processes, including supporting liver cell growth, metabolizing macronutrients, and even suppressing the development of liver cancer.
Research has also uncovered the direct impact that BCAA supplementation has on improving symptoms of hepatic encephalopathy. In a study examining patients with hepatic encephalopathy, oral ingestion of BCAAs mitigated neuropsychiatric symptoms. Another recent study revealed that supplementing hepatic encephalopathy patients with a combination of BCAAs and synbiotics (for gut bacteria health) improved cognitive function.
Some essential amino acids-particularly BCAAs- play a significant part in promoting skeletal muscle growth, improving metabolic functions, and reversing hyperammonemia.
Dietary Sources of Essential Amino Acids
Although continued studies are needed to determine exact molecular mechanisms, consuming food sources of amino acids may be key to protecting your liver and improving hepatic encephalopathy.
Essential amino acids are found primarily in protein-rich foods, which makes sense since proteins are comprised of amino acids on a basic molecular level. Sustained restriction of high-protein foods was once a common treatment for hepatic encephalopathy, but this guideline has been altered given the importance of proteins in counteracting malnutrition and providing essential amino acids.
Research shows that vegetable and dairy protein sources may be superior to animal protein in controlling ammonia levels and hepatic encephalopathy symptoms.
Dietary sources of essential amino acids that you can incorporate into your diet include:
| Lentils | Chickpeas |
| Lima beans | Soy protein products, like tofu |
| Chicken | Fish |
| Pumpkin seeds | Brown rice |
| Almonds | Quinoa |
| Cashews | Eggs |
Living with Liver Disease and Hepatic Encephalopathy
Hepatic encephalopathy is a highly complex condition and requires a similarly comprehensive and multifactorial treatment plan. A carefully planned nutritional regimen will compound the positive effects of a medical intervention, ultimately improving your prognosis and daily life. Remember, each person’s biochemistry is a little different and treatment plans must be individualized. Your doctor and dietician will ensure that your nutrition and lifestyle choices complement your medical treatment so you achieve the best possible outcome.