Hepatic encephalopathy is a condition that affects the brain and causes severe symptoms. If you’ve been diagnosed with hepatic encephalopathy, you may be wondering about the causes, symptoms, and treatment, as well as the hepatic encephalopathy life expectancy.
Read on to find out what you need to know about hepatic encephalopathy and associated liver diseases, as well as diagnosis, treatment, and prognosis.
What Exactly Is Hepatic Encephalopathy?
Hepatic encephalopathy is a complication of advanced liver disease that affects the brain. When liver function is severely compromised, the liver is unable to carry out its regular duties. One of these critical duties is metabolizing toxins to help protect the body from harm. In particular, the liver is responsible for converting ammonia into urea so that the kidneys can excrete it.
However, in advanced liver disease, liver function is compromised and is unable to convert ammonia into urea. As a result, ammonia levels build up in the bloodstream. High ammonia levels interfere with normal brain function.
Hepatic encephalopathy differs from metabolic encephalopathy because hepatic encephalopathy develops exclusively as a result of liver disease. Metabolic encephalopathy may develop as a result of dysfunction in other organs like the kidneys or a severe infection.
What are the symptoms of hepatic encephalopathy? Hepatic encephalopathy causes debilitating symptoms like confusion, speech impairment, personality changes, disorientation, coordination issues, extreme anxiety, and seizures. Hepatic encephalopathy often requires hospitalization.
Hepatic encephalopathy associated with liver disease may have specific triggers. For example, an episode of hepatic encephalopathy may be triggered by gastrointestinal issues like constipation. Constipation increases the absorption of ammonia that the liver cannot process, leading to hepatic encephalopathy symptoms.
There are many risk factors for developing liver disease, that may eventually lead to liver damage, complications of cirrhosis, and hepatic encephalopathy. Alcohol abuse causes significant inflammation in the liver, while the high consumption of sugar and saturated fat can cause nonalcoholic fatty liver disease. Common causes of liver damage include nonalcoholic fatty liver disease, alcoholic fatty liver disease, genetic conditions like hemochromatosis.
Co-Occurring Symptoms of Hepatic Encephalopathy
Because hepatic encephalopathy is a complication of liver disease, other symptoms and related complications of severe liver damage are usually also present.
- Ascites: Ascites is the accumulation of fluid within the abdominal Ascites may be associated with other serious complications, such as spontaneous bacterial peritonitis.
- Portal hypertension: When the liver is damaged, the portal vein in the liver may be under a significant amount of stress. Portal hypertension can lead to decreased blood flow to the liver and other complications like gastrointestinal bleeding and esophageal varices. Reduced blood flow through the liver causes more blood to flow through other veins, such as those in the esophagus. Esophageal varices are bulging veins in the esophagus.
- Hepatorenal syndrome: Portal hypertension can cause significant stress not only on the blood vessels in the liver but also in the renal blood vessels in the kidneys. Over time, the kidneys may be deprived of blood, causing significant damage.
- Jaundice: Jaundice describes yellowing of the skin and is associated with abnormally high levels of bilirubin in the body.
- Muscle wasting: Advanced liver disease prevents the body from processing and utilizing dietary nutrients effectively. As a result, the body breaks down its own muscle tissue, causing muscle wasting, fatigue, and weakness.
- Edema: Advanced liver cirrhosis can impede the flow of fluid through the body, leading to edema and swelling in the legs.
Diagnosing Liver Disease and Hepatic Encephalopathy Life Expectancy
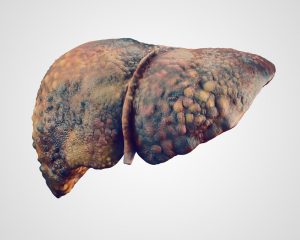
A severe case of hepatic encephalopathy indicates very advanced liver disease, end stage liver disease, or liver failure. The exact life expectancy and prognosis of liver disease and hepatic encephalopathy is best determined by your doctor. The presence of hepatic encephalopathy is a marker used in the Child-Pugh system and the Model for End-Stage Liver Disease, which helps doctors assess how advanced liver disease is and the prognosis for your specific case of liver disease.
The Child-Pugh system evaluates five factors: bilirubin levels, albumin levels, blood clotting time, ascites symptoms, and the presence of hepatic encephalopathy. Your Child-Pugh score then places you in a specific class based on the extent of liver damage.
The model for end-stage liver disease (MELD) score measures bilirubin levels, creatinine levels, and sodium levels. A higher MELD score is associated with more progressed liver damage.
Chronic liver disease may also be diagnosed using imaging techniques such as ultrasound, magnetic resonance imaging (MRI) scans, and computed tomography (CT) scans. These scans reveal abnormalities in the liver and detect liver conditions like cirrhosis, hepatocellular carcinoma, and inflammation. Blood tests can evaluate levels of ammonia, albumin, and liver enzymes.
Managing Hepatic Encephalopathy
Your case of liver disease will likely be managed by a team of healthcare professionals. Your team will include specialists in hepatology, gastroenterology, and radiology. If you have very late-stage liver disease or are hospitalized, nurses and caregivers will also be a crucial part of your treatment plan.
When liver disease is very advanced and liver function is severely compromised, such as in the case of end-stage liver disease and liver failure, a liver transplant is the best mode of treatment. Liver transplantation involves replacing diseased liver tissue with healthy liver tissue from a donor.
Cirrhotic patients may be prescribed medications like rifaximin, neomycin, and lactulose to manage the symptoms of hepatic encephalopathy. Rifaximin and neomycin are antibiotics that reduce the number of bacteria in the body that produce ammonia. Lactulose helps inhibit ammonia production in the gut.
You may also be prescribed other medications to manage other symptoms of liver disease. For example, diuretics may help reduce the fluid build-up in the abdomen as a result of ascites. If you suffer from hepatitis C or hepatitis B, you may be put on antiviral medications to help clear the infection.
You may also be advised to make changes to your diet. Eliminating alcohol is a crucial step in protecting remaining liver function. Eating an anti-inflammatory diet helps protect the liver from continued deterioration. Getting a balance of essential amino acids may be necessary for supporting the balance of amino acids in the brain and supporting increased muscle mass. Always consult your healthcare provider about diet changes and supplements.
Hepatic Encephalopathy Life Expectancy: Conclusion
Hepatic encephalopathy is a severe complication of advanced liver disease. Prognosis, mortality rate, and life expectancy can vary based on your specific case of liver disease. However, medical interventions can help improve your health-related quality of life and manage hepatic encephalopathy symptoms and liver disease.