If you have fatty liver disease, there’s a good chance that you are also experiencing symptoms of heartburn on a regular basis. Here we discuss heartburn vs acid reflux, and when acid reflux becomes gastroesophageal reflux disease. Having chronic heartburn can be extremely painful and affect your daily life. You may be wondering what you can do about the unpleasant symptoms of heartburn. Luckily, there are steps you can take to help relieve acid reflux associated with fatty liver disease, so you can increase your quality of life.
What’s Happening When You Feel Heartburn?
When we eat, chewed food is funneled down the esophagus toward the stomach. The connection between the esophagus and stomach is modulated by the esophageal sphincter, which is a ring of muscle that can relax and contract. The esophageal sphincter is able to let food make its way from the esophagus to the stomach, while also preventing the backflow of stomach acid into the esophagus.
Acid Reflux Causes Heartburn
What is stomach acid? Stomach acid is the caustic acid – hydrochloric acid – used to chemically break down the foods you eat and help get rid of any harmful viruses and bacteria. The lining of your stomach is designed to handle this acid. On the other hand, your esophagus is designed to facilitate the passage of food into the stomach and is not meant to handle acidic substances. If the esophageal sphincter isn’t working as well as it should, stomach acid is not effectively contained within the stomach. The acid will flow backward and irritate the esophagus, in a process known as acid reflux or gastroesophageal reflux. Acid reflux is the mechanism that causes the painful burning sensation known as heartburn.
What Does Heartburn Feel Like?
The sensation of heartburn feels precisely as the term describes- like your heart is burning. Your heart, however, is not burning. The placement of the esophagus on the left side of your chest, near your heart, can create such a sensory illusion. This sensation can also extend through upper parts of the esophagus, causing a burning feeling towards the back of your throat.
Other Symptoms of Acid Reflux
Is heartburn the only symptom, or can acid reflux cause nausea and other symptoms as well? Though heartburn is often the primary, most unpleasant symptom of acid reflux, you may also be experiencing additional related symptoms such as nausea.
Some of the most common symptoms of acid reflux, in addition to heartburn, include:
- Nausea
- Vomiting
- Unrelenting hiccups
- Sore or scratchy throat
- Difficulty swallowing
- Coughing
- Trouble with swallowing
- Bad breath or bad taste in the mouth
- Regurgitation, or stomach fluids traveling upwards through the esophagus, sometimes into the mouth
- Chest pain
- Pressure or pain in the stomach
When It’s Gastroesophageal Reflux Disease
Occasional heartburn symptoms can be normal, such as after a large, high-fat meal. However, regular bouts of acid reflux can severely impact your quality of life. When you experience chronic acid reflux several times a week or more, you may have a condition called gastroesophageal reflux disease (GERD).
How is GERD diagnosed? The symptoms of GERD are the same as those experienced with acid reflux disease. Your doctor will be able to determine whether you have GERD by assessing your symptoms, checking how well your esophageal sphincter functions. An endoscopy involves examining the inside of the stomach and esophagus with a tiny camera, allowing your physician to evaluate your digestive function and presence of acid reflux. The type of specialized physician who deals mainly with stomach-related illnesses is a gastroenterologist.
Your doctor may also conduct an esophageal potential of hydrogen (pH) test. A pH test can reveal the acidity of certain body tissues and fluids. A pH of 7 indicates a neutral environment, and a pH lower than 7 indicates an acidic environment. The pH of stomach acid ranges between 1 and 5. If the pH of the esophagus reaches 4, this may indicate the presence of stomach acid. (1)
Your doctor will also be able to assess whether your symptoms are a primary result of acid reflux or the result of another medical condition such as a hiatal hernia.
So, how long does GERD last? If left untreated, GERD can last for years and lead to severe complications.
Complications
If acid reflux or gastroesophageal reflux disease is left untreated for a long period of time, it can lead to several complications.
- Esophagitis: Chronic damage to esophageal cells can result in inflammation of the esophageal lining. This may result in bleeding and the growth of ulcers. Over time, scar tissue may develop in the esophagus and impede the passage of food into the stomach.
- Barrett’s Esophagus: Chronic exposure to stomach acid can alter the structure and development of cells in the esophagus. In some cases, Barrett’s esophagus may increase the risk of developing cancerous cells that progress to esophageal cancer.
- Esophageal Cancer: When stomach acid consistently damages tissue in the esophagus, esophageal cells must constantly work on repairing. Over time, malignant cells may develop and proliferate, resulting in esophageal cancer.
Why Do You Experience Heartburn with Fatty Liver?
Moreover, research shows a direct connection between nonalcoholic fatty liver disease and acid reflux. There is a significant correlation between the presence of gastroesophageal reflux disease and fatty liver disease. (2, 3)
But what is the reason for co-occurring acid reflux and fatty liver disease? Most likely, the common causal factor is metabolic syndrome. Just as science has shown the link between metabolic syndrome and fatty liver disease, research has also revealed the connection between metabolic syndrome and acid reflux. (4)
Metabolic syndrome encompasses a wide array of conditions, including high blood pressure, high LDL cholesterol, low HDL cholesterol, type 2 diabetes, obesity, and insulin resistance. Diet and lifestyle factors that contribute to metabolic syndrome also contribute to acid reflux and fatty liver disease.
Heartburn with Alcohol-Induced Fatty Liver Disease
Alcoholic fatty liver disease can increase the risk of experiencing heartburn. Chronic alcohol intake aggravates the stomach and stimulates acid production and weakens the esophageal sphincter. On top of that, alcohol can further disrupt the delicate balance of gut flora in the digestive system, which can cause associated symptoms of digestive discomfort.
The Role of Inflammation in Heartburn
Beyond food, the body’s inflammatory response may contribute to acid reflux. A study published in the Journal of the American Medical Association suggested that an inflammatory immune response through cytokines plays a role in esophageal damage, instead of acid-induced damage. (5)
It makes sense that inflammation may be a culprit in the development of acid reflux. Systemic inflammation is a common state that both contributes to and results from both metabolic syndrome and fatty liver disease.
Inflammation describes a type of activated immune response. When inflammation is acute, the immune system is responding to an injury or invading pathogen. Acute inflammation is an adaptive mechanism that helps the body heal and recover from illness. When the immune system has done its job and a wound is healed or an infection is eliminated, the immune system can retreat and inflammation resolves.
On the other hand, chronic inflammation is a maladaptive mechanism in which the immune system is constantly overactivated. On a molecular level, this can be described as the presence of inflammatory cells like lymphocytes, macrophages, and cytokines throughout the body. (6)
Oxidative stress contributes to inflammation as well. When the body is exposed to pollutants, allergens, or highly processed foods with added chemicals, tissues are unable to function as usual. Waste products and reactive free radicals accumulate in cells, inflicting mitochondrial damage and impeding normal metabolic processes.
Over time, chronic inflammation and oxidative stress damage tissues and inhibit your organs from carrying out their duties effectively. If left unresolved, inflammation can cause or exacerbate conditions like metabolic syndrome, cardiovascular disease, fatty liver disease, and acid reflux.
What You Can Do if You Have Acid Reflux and Fatty Liver Disease
If you have both acid reflux and fatty liver disease, there is a high chance that the two conditions are linked. Therefore, steps for reversing fatty liver disease will also effectively lower the incidence of acid reflux.

Decreasing Systemic Inflammation
The central pillar of eliminating acid reflux is following a diet and lifestyle that lowers inflammation.
1. Stay Away from Refined Carbohydrates
The digestive system quickly converts refined carbohydrates into sugar, which spikes your blood glucose. Consuming refined carbohydrates can over time contributes to the development of insulin resistance and type 2 diabetes, as well as weight gain and fatty liver disease. The key to decreasing inflammation is avoiding refined carbs like white bread, white pasta, and white rice. Even though these foods are typical lunch and dinner foods, the body handles refined grains like sugar. Other examples of refined carbs include soda, candy, sugary breakfast cereals, cookies, cakes, ice cream, and any product with added sugar.
2. Avoid Processed Meat and Dairy Products
Processed meat and dairy products are often high in saturated fat, which contributes to inflammation and cardiovascular disease. These products also tend to contain added preservatives and sodium which can trigger inflammatory reactions and raise blood pressure. Moreover, trimethylamine N-oxide is an inflammatory byproduct of digesting animal products that contributes to systemic inflammation. To help quell inflammation, steer clear of foods like lunch meats, ground beef, steak, chicken, and cheese.
However, eating controlled portions of fresh meats and yogurt low in saturated fat provide high-quality protein and optimal ratios of amino acids. If you’re going to consume animal products, stick to fresh fatty fish like salmon which is also high in omega-3 fatty acids, which is a healthy kind of fat that helps reduce inflammation. Low-fat, sugar-free Greek yogurt is another nutritious choice. Yogurt contains protein and probiotics that support digestive health.
3. Eat Mainly Whole, Plant-Based Foods
Whole, plant-based foods are rich in vitamins, minerals, antioxidants, fiber, healthy fats, and other nutrients that promote healing and banish inflammation. Whole foods are also free of irritating preservatives or other added chemicals, while also containing prebiotics that promote digestive health. Whole grains, vegetables, and fruit afford fiber and antioxidants as well as complex carbohydrates that help your body sustain energy. Beans and nuts provide healthy fats and protein. When possible, buy organic produce or thoroughly rinse produce to avoid consuming pesticides that may aggravate the digestive system. Below are excellent options in each category that will boost your immune system, help eradicate inflammation, and support digestive health.
- Whole grains: Excellent options for whole grains include quinoa, brown rice, millet, oats, whole-grain pasta, amaranth, and farro. When choosing whole grains, it’s critical to making sure that the grains are as unprocessed as possible. This means that the grain retains its nutrient-rich husk, and therefore contains higher concentrations of protein, fiber, antioxidants, and vitamins.
- Fruits: Delicious and nutritious fruit options include apples, bananas, cherries, blueberries, raspberries, strawberries, guava, watermelon, kiwi, and papaya. There are often questions surrounding whether the sugar in fruit is healthy or detrimental. The answer is that the sugar naturally present in whole fruits is perfectly healthy. The body processes naturally occurring sugar much differently than added sugars. When consumed in a package of fiber, vitamins, and antioxidants, the sugar present in whole fruit is digested slowly and doesn’t spike your blood sugar.
- Vegetables: Vegetables contain high levels of antioxidants, fiber, and vitamins. Excellent vegetable options include sweet potatoes, kale, broccoli, spinach, carrots, beets, brussels sprouts, squash, and eggplant.
- Beans: Beans contain protein and fiber and help you fill up when focusing on plant-based whole foods. Nutritious bean options include lentils, black beans, cannellini beans, kidney beans, soybeans or edamame, lima beans, and black-eyed peas.
- Nuts and seeds: Nuts and seeds are filled with healthy fats, fiber, protein, and antioxidants that fight inflammation. Try adding almonds, walnuts, pumpkin seeds, flax seeds, and chia seeds to your diet.
4. Maintain a Healthy Weight
Carrying excess body weight exacerbates inflammation and increases the risk of high cholesterol, high blood pressure, fatty liver disease, and acid reflux. If you are overweight, reduce your caloric intake to support your ideal weight based on your body frame and height. Additionally, losing weight may be particularly critical if you tend to carry weight in your abdomen. Excess fat accumulated around the stomach and other organs can exert pressure on the esophageal sphincter. This can weaken the esophageal sphincter and cause it to open, which leaves an open path for stomach acid and other stomach contents to backflow into the esophagus and mouth.
5. Reduce or Cut Out Alcohol
Alcohol, in addition to irritating the stomach, causes systemic inflammation. Organs that are particularly impacted include the liver, brain, pancreas, and stomach. The cells throughout your body must work hard to metabolize and detoxify alcohol, and these processes get in the way of normal cellular function. To minimize alcohol-induced inflammation, try eliminating alcohol or at least limiting your consumption.
6. Exercise
Exercise strengthens your body’s cardiovascular system, fights inflammation, and helps reverse and prevent metabolic syndrome. Exercise also helps to maintain a healthy weight by burning calories. Incorporating aerobic exercise and strength training into your lifestyle will help you lose weight while maintaining muscle mass. Ultimately, exercise plays a role in reversing fatty liver disease and calming systemic inflammation.
How to Individualize Your Diet Plan if You Have Heartburn
An anti-inflammatory diet and lifestyle provide an excellent foundation for combatting acid reflux disease naturally. After that, it’s critical to then tailor your diet to help decrease stomach acid and avoiding triggers. There’s no one-size-fits-all when it comes to the diet for heartburn. Individuals with acid reflux have unique biochemistries and subsequent sensitivities that result in a heartburn flare.
Always be mindful of the foods you eat and observe if heartburn episodes seem connected to a certain food. It may help to keep a food diary to make it easier to assess patterns.
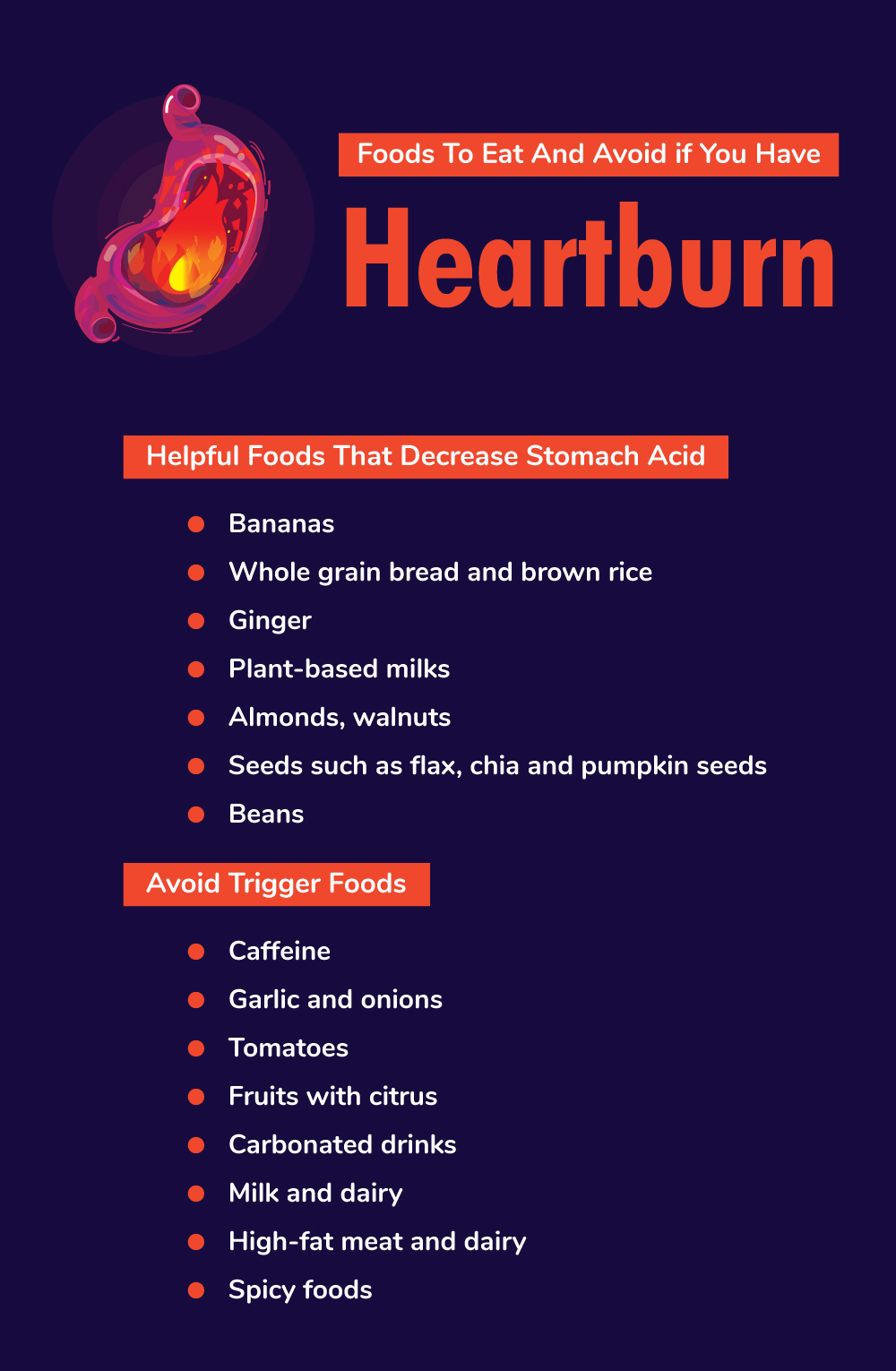
Helpful Foods That Decrease Stomach Acid
Foods that are non-acidic, also referred to as alkaline, will help calm the stomach and prevent heartburn.
Examples of alkaline foods include:
- Bananas: Bananas are well known for soothing the stomach, and they’re also rich in
- Bread and rice: These carbohydrates help calm the stomach. Just make sure you go for the whole-grain bread and brown rice.
- Ginger: This ancient herb has long been regarded as a therapeutic agent for the digestive system.
- Plant-based milks: Along with water, plant-based milks are generally neutral and soothe the stomach.
Avoid Trigger Foods
Though triggers may vary depending on the person, there are some common trends when it comes to the foods that worsen acid reflux.
Once you’ve identified your specific triggers, cross those off your grocery list. In the meantime, steer clear of these foods to help avoid a heartburn episode:
- Caffeine: Caffeine in coffee or tea is a stomach irritant and may contribute to heartburn.
- Garlic and onions: For some people, compounds in garlic and onions are difficult to digest and may cause heartburn.
- Tomatoes: Tomato is a fruit that is high in acid, which can irritate the stomach and cause heartburn. Try eliminating fresh tomatoes as well as tomato products like tomato soup, canned tomatoes, and ketchup.
- Fruits with citrus: Citrus fruits contain citric acid, which may trigger acid reflux. Try avoiding oranges, grapefruits, lemons, limes, and tangerines.
- Carbonated drinks: Try cutting out all carbonated drinks, like soda. Carbonation can release excess gas and cause the esophageal sphincter to weaken and open.
- Milk and dairy: For some people, digesting milk and dairy products can be difficult and bring on heartburn.
- High-fat meat and dairy: Try avoiding fatty foods like meat and dairy products, which not only increase inflammation but also are difficult for the stomach to digest.
- Spicy foods: Try avoiding foods that are heavily seasoned with strong spices like chili pepper and red pepper. These may irritate the stomach and cause an episode of acid reflux.
Other Helpful Tips for Decreasing Acid Reflux Symptoms
- Avoid eating right before going to sleep. Eating a meal and then directly lying down to sleep may trigger acid reflux, which can disrupt your sleep. Allow several hours for digestion before going to bed.
- Eat smaller meals. Instead of eating one huge meal, try eating small meals more frequently or snacking throughout the day. A large meal requires more stomach acid for digestion, which increases the likelihood that acid will creep up the esophagus. A large volume of food in the stomach can also place pressure on the esophageal sphincter which may cause it to open, allowing food to acid to backflow. On the other hand, smaller meals require less stomach acid and don’t put pressure on the esophageal sphincter.
- Stay upright after eating. By remaining upright after eating, you can take full advantage of gravity’s ability to keep food and acid where they belong – in the stomach. Try taking a gentle walk or standing until food has comfortably digested.
Other Interventions
A number of over-the-counter medications help manage the symptoms of heartburn. For example, Tums is an antacid that helps neutralize stomach acid. Proton-pump inhibitors (PPIs) like Nexium or Prilosec treat heartburn by decreasing the amount of stomach acid your body produces. Your doctor can also assess the medications that you may be taking for other conditions, since some medicines may increase the risk of acid reflux. If you have another underlying condition that is contributing to acid reflux, always consult your doctor on medical interventions to treat the condition.
Sometimes, the symptoms of heartburn and a heart attack can be confused, if you are unsure and haven’t experienced heartburn before, always seek medical attention.
Conclusion
In summary, having fatty liver disease increases the risk of experiencing heartburn, acid reflux, and gastroesophageal reflux disease. Dietary and lifestyle changes that aim to reduce inflammation will be effective in both reversing fatty liver disease and preventing acid reflux.
References:
(1) https://www.nature.com/gimo/contents/pt1/full/gimo31.html
(2) https://www.ncbi.nlm.nih.gov/pubmed/31338830
(3) https://www.ncbi.nlm.nih.gov/pubmed/24718860
(4) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5292393/
(5) https://jamanetwork.com/journals/jama/fullarticle/2521970