Weight loss surgery is growing in popularity as a treatment for obesity and related metabolic conditions like type 2 diabetes and nonalcoholic fatty liver disease. Both gastric sleeve surgery and gastric bypass surgery are forms of bariatric surgery, though they also exhibit a few significant differences that you may want to consider when deciding which form of surgery you should get. Being equipped with information is the key to making sure you’re choosing the form of bariatric surgery that best fits your specific needs. In this article, you’ll learn about the similarities and differences between gastric sleeve vs gastric bypass surgery.
Types of Weight Loss Procedures: Gastric Sleeve and Gastric Bypass
There are several variations of bariatric surgery, though typically patients receive either gastric sleeve surgery or gastric bypass surgery. Gastric sleeve and gastric bypass are sometimes referred to as forms of metabolic surgery since they help instigate weight loss and improve metabolic conditions.
Anatomy of the Digestive System
Let’s first take a look at the anatomy of the digestive system. Having a grasp of the mechanisms behind digestive function helps us understand how bariatric surgery helps facilitate weight loss.
Normally, the stomach is shaped like a large rounded pouch that is connected to the esophagus. As food enters the stomach, hydrochloric acid helps break down food particles to create a mixture called chyme.
The stomach then empties into the upper part of the small intestine, called the duodenum. In the duodenum, enzymes from the pancreas and bile fluid help to break down bonds in proteins and fats. Food particles are then channeled into the next section of the intestine, called the jejunum, where the intestinal lining absorbs macronutrient particles including sugar molecules, individual amino acids, and fatty acid chains. The last section of the small intestine is called the ileum and absorbs micronutrients like vitamins and minerals.
Our appetite and the amount of food we eat is moderated by a balance of hormones called ghrelin and leptin. Ghrelin is produced in the stomach lining and sends signals to the brain, resulting in the sensation of hunger. Leptin, on the other hand, is secreted by fat stores in the body and sends signals to the brain that signify that the body is nourished, which decreases appetite. Obesity interferes with the normal mechanisms of ghrelin and leptin.
Gastric Sleeve vs Gastric Bypass Surgery
Both the gastric sleeve and gastric bypass surgeries physically alter the digestive system to influence food intake, resulting in weight loss. However, several differences distinguish the procedures from one another.
Differences
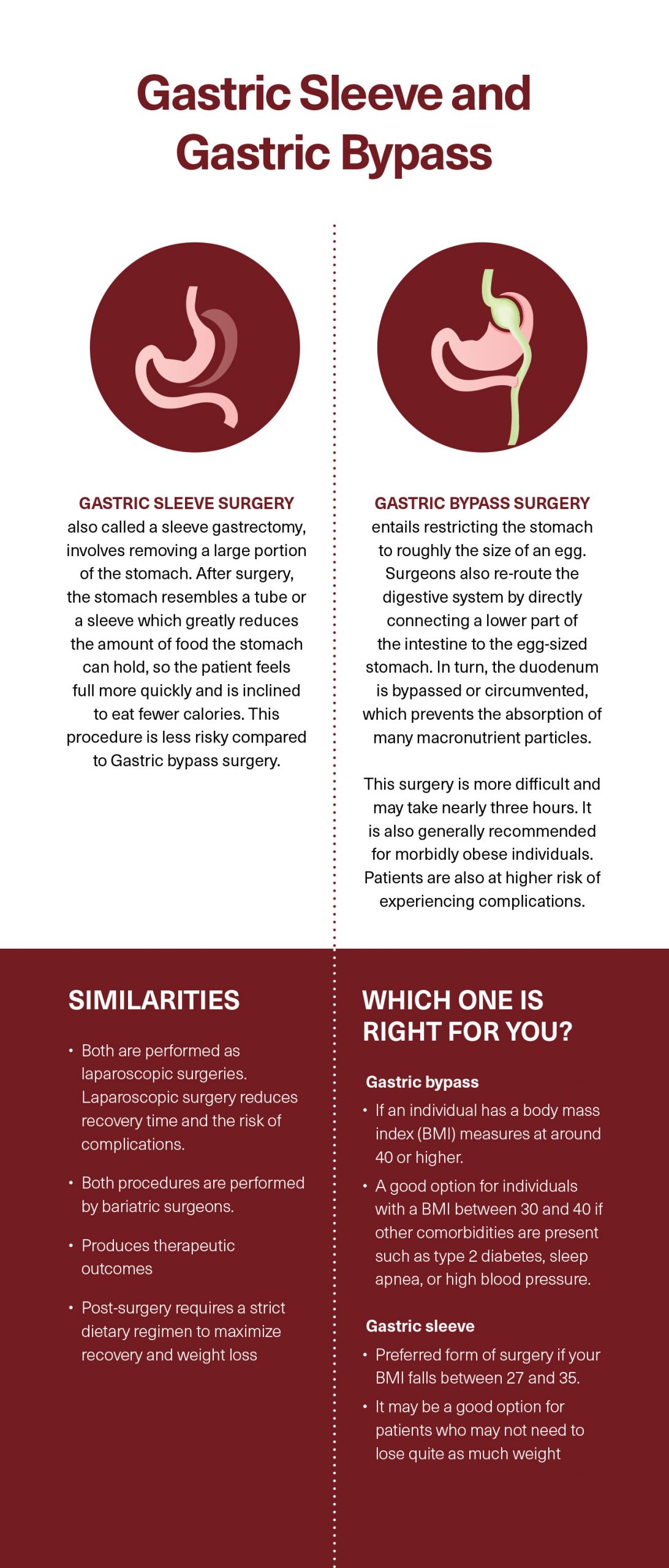
The gastric sleeve surgery also called a sleeve gastrectomy, involves removing a large portion of the stomach. After surgery, instead of resembling a curved pouch, the stomach instead resembles a tube or a sleeve. This tube-like shape greatly reduces the amount of food the stomach can hold, so the patient feels full more quickly and is inclined to eat fewer calories. The stomach after gastric sleeve surgery also serves as a tunnel that directly funnels food particles from the esophagus to the duodenum.
Gastric sleeve surgery also has hormonal implications. By removing such a significant portion of the stomach, less stomach lining is available to excrete ghrelin. With significantly lower levels of ghrelin production, the patient receives fewer hunger signals and therefore eats less food.
A variation of the gastric sleeve procedure is available, in which the gastric sleeve tactic is combined with a duodenal switch. Performing a duodenal switch means that much of the duodenum is removed in addition to the stomach, meaning fewer caloric nutrients can be absorbed. This state is called malabsorption and decreases the caloric impact of foods consumed.
Gastric bypass surgery, most commonly performed as the Roux-en-Y gastric bypass, has been performed for many decades and was developed as a form of weight loss procedure before the gastric sleeve surgery. Performing gastric bypass entails restricting the stomach to roughly the size of an egg. Surgeons also re-route the digestive system by directly connecting a lower part of the intestine to the egg-sized stomach. In turn, the duodenum is bypassed or circumvented, which prevents the absorption of many macronutrient particles. Because of stomach size has been decreased to become a small pouch, gastric bypass effectively provokes weight loss by reducing food consumption. The reduction in stomach lining also lowers ghrelin hormone production and increases leptin production, helping to improve the function of appetite-regulating hormones.
Similarities
Though historically gastric sleeve and gastric bypass were open surgeries, today they are performed as laparoscopic surgeries. In contrast to open surgery, laparoscopic surgery entails the use of surgical instruments and cameras that reach the stomach through tiny cuts in the skin. Laparoscopic surgery reduces recovery time. It also reduces the risk of complications by protecting inner organs from exposure to open air.
Both procedures are performed by bariatric surgeons. Specialized surgeons in bariatric procedures have completed a residency in general surgery followed by a fellowship in bariatric surgeries.
Finally, both gastric sleeve and gastric bypass produce therapeutic outcomes. Patients who undergo either procedure lose a majority of their excess weight within the first year after surgery. Patients also see marked improvements in health conditions associated with obesity.
Researchers at the Oregon Health & Science University and the University of Colorado School of Medicine analyzed the outcomes for patients undergoing bariatric surgery. (1) Results showed improvements in comorbidities associated with obesity, including sleep apnea, cardiovascular health, and nonalcoholic fatty liver disease. Bariatric surgery was also shown to be a successful intervention for prediabetes, significantly reducing the incidence of type 2 diabetes among patients. The impacts of bariatric surgery for mitigating high blood pressure are less clear. Interestingly, results showed that though bariatric surgery was effective for reducing fat accumulation for patients with early stages of fatty liver disease, it was not effective for reducing liver inflammation associated with nonalcoholic steatohepatitis. (1)
Weight Loss Surgery Requirements for Gastric Sleeve and Gastric Bypass: Which One Is Right for You?
Weight loss surgery is reserved for patients as a last resort to losing weight. Before turning to weight loss surgery, an individual should exhaust all possible dietary, lifestyle, and medical options for achieving weight loss.
The specific requirements for gastric sleeve procedure and gastric bypass vary. Gastric bypass is a more difficult and involved procedure and is generally recommended for morbidly obese individuals whose body mass index (BMI) is measured at around 40 or higher. A surgeon may also deem gastric bypass to be a good option for individuals with a BMI between 30 and 40 if other comorbidities are present such as type 2 diabetes, sleep apnea, or high blood pressure.
The gastric sleeve procedure is generally less risky and is the preferred form of surgery if your BMI falls between 27 and 35. The gastric sleeve procedure may be a good option for patients who may not need to lose quite as much weight, though both procedures lead to significant weight loss and improvements in metabolic conditions.
Make sure to discuss your options with your surgeon, who will present all the information and choose the best form of surgery for your weight and health conditions.
Preparing for Weight Loss Surgery
The preparation process for weight loss surgery is rigorous and involves medical evaluation, psychological evaluation, and lifestyle changes. These guidelines are critical to the success and safety of the weight loss procedure that you undergo.
The treatment team for bariatric surgery pre-operative care involves dieticians, psychologists, and physicians. Obese patients inherently face higher risks during operations in comparison to patients with a BMI within a normal range. Medical evaluations allow the doctors to evaluate your current health status and suitability for surgery. Testing may include blood tests to evaluate cholesterol levels, liver function, and kidney function. Your physician may also administer a stress test and electrocardiogram (EKG) to evaluate your cardiovascular health and whether your heart can withstand surgery.
Physicians often require several months of pre-operative preparation during which patients re-establish eating patterns and lifestyle habits. If medical imaging reveals that your liver is enlarged, physicians also prescribe a very low-calorie, low-carb diet that helps shrink your liver to more normal size. An enlarged liver indicates the presence of nonalcoholic fatty liver disease and inflammation. During surgery, having an enlarged liver can be very dangerous and raise the risk of encountering serious complications during surgery, such as excessive bleeding.
Dietitians are a vital part of helping patients implement a healthy diet that balances macronutrients and provides a variety of micronutrients that help lower inflammation, lower blood sugar levels, and initiate weight loss. In addition to providing food guidelines for pre-surgery preparation, dietitians may also suggest supplements to optimize your health before surgery.
Therapists and psychologists can help patients address any cognitive or psychological factors that may be contributing to stress, overeating, binge eating, and other unhealthy eating patterns.
Establishing a routine, addressing underlying issues, and initiating weight loss before undergoing surgery reduces the risk of physical complications associated with surgery. Moreover, intensive pre-operative preparation ensures that patients are prepared to continue lifestyle and nutrition patterns that complement surgical interventions, maximizing, and sustaining long-term benefits.
How Long Does Gastric Bypass Surgery Take?
Gastric bypass surgery requires significantly more time in the operating room than the gastric sleeve surgery overall. A gastric bypass procedure may take nearly three hours, while it takes about half of that time to perform a gastric sleeve procedure. However, it’s important to keep in mind that operating time will vary considerably based on each individual patient. For example, BMI may be a factor in operating time. Research conducted at Stanford University Medical Center revealed that a higher BMI was correlated with longer operating times during bariatric surgery. (2)
Risks and Potential Complications Associated with Bariatric Surgery
Before pursuing a surgical procedure for weight loss, it’s important to be aware of potential risks and any complications that could occur. In comparison to complications after gastric sleeve surgery, patients are at a higher risk of experiencing complications following gastric bypass surgery. Gastric sleeve complications are still possible, however, and can be similar to gastric bypass complications.
Below are a few of the possible complications that could accompany bariatric surgery.
- Gallstones: Rapid weight loss can precipitate the formation of gallstones, which may need to be surgically removed. Symptoms of a gallstone may include sudden, sharp pain in the back, below the sternum, or in the upper right quadrant of the abdomen. Gallstone pain is sometimes mistaken for liver pain since the gallbladder and the liver are next to one another. Sharp pains may be accompanied by nausea and vomiting.
- Blood clots: Being stationary during surgery and the recovery period increases the risk of experiencing a blood clot. Also called deep vein thrombosis, blood clots are most likely to develop in the legs. If the blood clots travel, they have the potential to block blood flow in blood vessels, depriving tissues, and organs of oxygen and precipitating cell death. Blood clots can cause serious issues such as a pulmonary embolism, which cuts off blood supply to the lungs. To effectively avoid a blood clot, start moving around as soon as possible after surgery to keep your blood from pooling.
- Infection: As with any wound, infection is possible after surgery. Make sure to keep the surgical site clean and follow all instructions for taking care of wounds post-surgery. In some cases, an infection may develop internally. Usually, you will receive a course of antibiotics immediately following surgery to keep any potential infection at bay. A healthy, balanced diet that is low in added sugar and high in vitamins and antioxidants can also help your immune system prevent infection.
- Dumping syndrome: Dumping syndrome describes the condition in which ingested food moves too rapidly from the stomach to the intestines. Dumping syndrome usually occurs in response to eating processed and refined foods that are high in added sugars, saturated fats, and sodium. An individual may experience these symptoms within half an hour of eating a meal, or several hours after. Early dumping produces different symptoms than late dumping. Symptoms of early dumping syndrome include nausea, cramps, diarrhea, vomiting, fast pulse, bloating, and the sensation of being too full. Late dumping exhibits primarily as weakness, lightheadedness, sweating, and a fast heart rate. Though dumping syndrome is no fun, at the same time, experiencing these symptoms may have a silver lining. Since it is an unpleasant experience, you may begin to associate junk food with the symptoms of dumping syndrome, which can prove to be an effective deterrent from eating delicious but unhealthy foods like cookies, cakes, potato chips, fries, ice cream, and cheeseburgers.
- Acid reflux: Acid reflux, or gastroesophageal reflux disease (GERD), is commonly associated with obesity, but can also be triggered after bariatric surgery. GERD is a common complication after weight loss surgery since a small stomach makes it easier for stomach acid to make its way into the esophagus. The symptoms of GERD involve a burning sensation in the chest or throat that is better known as heartburn. You may also experience stomach pain. Diet will play a role in mitigating symptoms of GERD. Stay away from high-fat, high-sugar foods that may exacerbate acid reflux.
- Nutrient deficiencies: Following bariatric surgery, food consumption is restricted and much of the small intestine responsible for nutrient absorption has been removed. Low food intake combined with a malabsorptive digestive system increases the risk of developing nutrient deficiencies. Make sure to carefully follow the nutrition plan mapped out by your physician and dietician. One of the most common deficiencies is protein deficiency. Read below to find out how to best combat protein deficiency following bariatric surgery.
Keep in mind that serious complications are rare, but it’s good to be vigilant about any concerning symptoms or side effects that persist after surgery. If you experience a fever, severe pain, vomiting, chills, or any other worrisome symptoms, seek medical attention immediately.
Recovering from Gastric Bypass and Gastric Sleeve
Both gastric sleeve and gastric bypass patients must follow a strict dietary regimen following surgery, in order to maximize recovery and weight loss. In both cases, the amount of food you can eat will be significantly restricted.
While the stomach and digestive system heal, you will likely be in the hospital for a few days following the procedure. In the hospital, the doctors and nurses will monitor your progress, bring you liquids, and prepare you to implement your post-surgery nutrition plan when you go home. Health care workers will also encourage you to take regular walks through the hospital as soon as you are able, to help prevent the development of blood clots.
Nutrition After Gastric Sleeve or Gastric Bypass
A healthy diet and balanced lifestyle patterns are critical to the long-term success of bariatric surgery.
In a review published in Advances in Nutrition, researchers in Israel compiled nutritional recommendations and guidelines used in clinical practice for adults receiving weight loss surgery. (3) Though your individualized nutrition recommendations will be made at your doctor’s discretion, a general timeline of nutrition post-surgery will progress as described: (3)
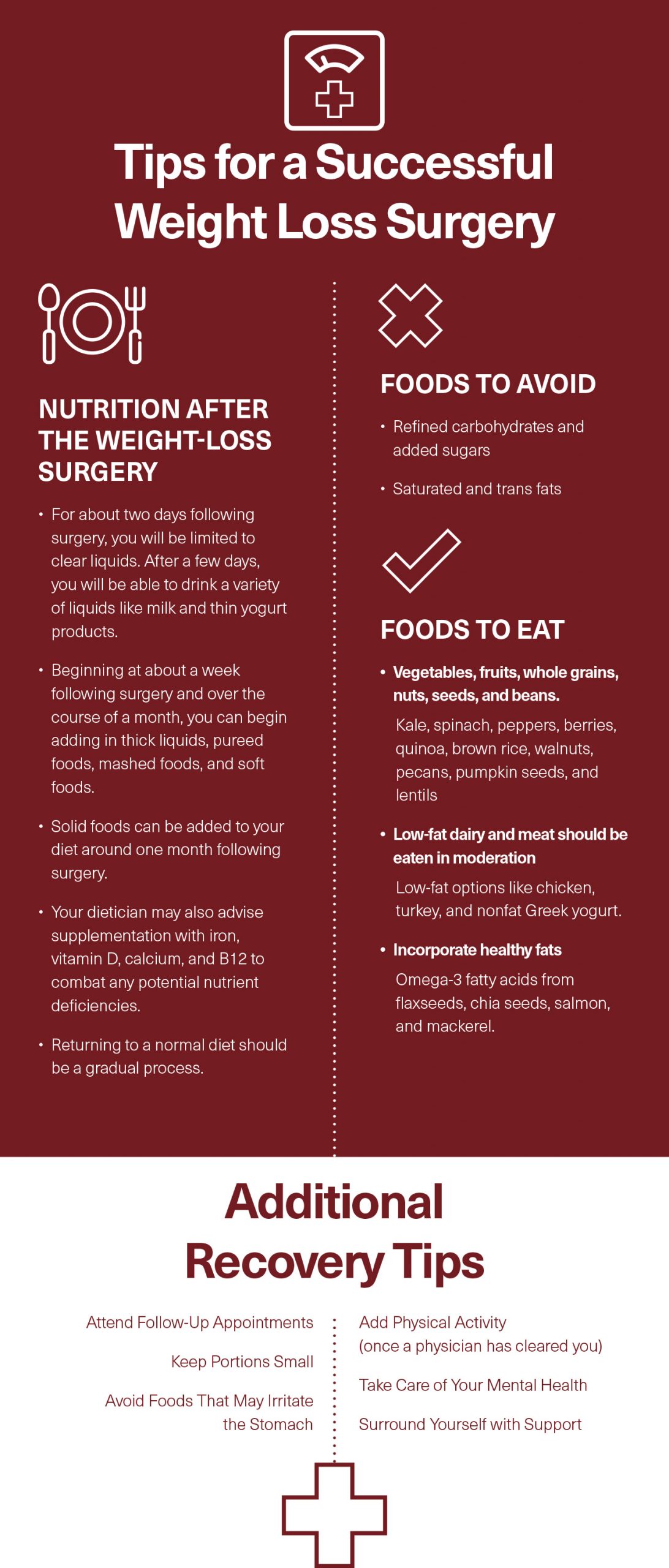
For about two days following surgery, you will be limited to clear liquids. After a few days, you will be able to drink a variety of liquids like milk and thin yogurt products. Beginning at about a week following surgery and over the course of a month, you can begin adding in thick liquids, pureed foods, mashed foods, and soft foods as your physician and dietitian deem appropriate for your individual case.
When approved, good examples of healthy foods that can be pureed and mashed include sweet potatoes, yogurt, low-sugar pudding, cottage cheese, avocado, cottage cheese, and soft eggs. Other soft foods include ground meats, soft cheese, and cooked vegetables like cauliflower, carrots, broccoli, and zucchini. Soft fruit options include mango, strawberry, guava, apples, and papaya. Just make sure that all fruits and vegetables have the peel removed since peels are more fibrous and difficult to digest.
Solid foods can be added to your diet around one month following surgery. Try adding cooked black beans, kidney beans, split peas, and whole-grain bread to your diet. After two months, all foods of varying textures can be incorporated into your diet.
Your dietician may also advise supplementation with iron, vitamin D, calcium, and B12 to combat any potential nutrient deficiencies. Iron and B12 supplements will prevent anemia, while vitamin D and calcium will ensure efficient immune response while decreasing inflammation and fortifying your bones and muscle tissue. You will likely also be prescribed a multivitamin to supplement your diet.
Returning to a normal diet should be a gradual process. When you return to a normal diet, your portion sizes will need to remain small to prevent stretching and damage in the stomach and digestive system. It’s also crucial to maintain a healthy diet in order to reap all the benefits of weight loss surgery and decrease the likelihood of experiencing complications.
Foods to Avoid
Staying away from certain foods while choosing the right ones will help prevent gastric reflux symptoms, lower inflammation, reduce recovery time, and help you get rid of excess weight and metabolic conditions for good.
- Refined carbohydrates and added sugars: Stay away from refined carbohydrates and added sugars, which increase the risk of developing dumping syndrome and also contribute to weight gain, insulin resistance, type 2 diabetes, and fatty liver disease. Refined carbohydrates include any product that contains grain that has been processed to remove nutritional factors. Examples of refined carbohydrates include white bread, white rice, white potato products, boxed cereals, chips, crackers, cookies, cakes, and other baked goods. Foods that likely include added sugars are granola bars, candy, yogurts, salad dressings, white breads, cookies, and other baked goods.
- Saturated and trans fats: Saturated fats found in fried foods, meat, and dairy products increase the risk of insulin resistance, weight gain, and fatty liver disease. Steer clear of high-fat steaks, dark meat chicken, bacon, whole milk, cheese, French fries, fried chicken, and burgers.
Foods to Eat
Your diet after gastric bypass surgery should be rich in whole foods. The Mediterranean diet provides excellent guidelines for foods that should be incorporated into your diet. A plant-focused Mediterranean diet is extremely effective for supporting weight loss, maintaining healthy cholesterol levels, reversing diabetes, reversing fatty liver disease, improving recovery time, and restoring metabolic health and cardiovascular health.
The base of your diet should be made of vegetables, fruits, whole grains, nuts, seeds, and beans. Antioxidant-packed plant foods help reverse inflammation. Kale, spinach, peppers, berries, quinoa, brown rice, walnuts, pecans, pumpkin seeds, and lentils are examples of plant-based foods that support your health. Low-fat dairy and meat should be eaten in moderation but can be important sources of protein and essential amino acids following weight loss surgery. Stick to low-fat options like chicken, turkey, and nonfat Greek yogurt. Incorporate healthy fats like omega-3 fatty acids into your diet from flaxseeds, chia seeds, salmon, and mackerel.
Combatting Protein Deficiency
Protein deficiency is a common occurrence following bariatric surgeries like gastric sleeve and gastric bypass. (3) Be on the lookout for symptoms of protein deficiency such as exhaustion, hair breakage, slow recovery from illness, dry skin, muscle wasting, brain fog, and mood swings.
Though surgery-induced malabsorption and the restrictions on food intake and ultimately lead to weight loss and positive outcomes for metabolic conditions, they also commonly lead to protein deficiency. Low protein intake means that you are not consuming an adequate amount of essential amino acids that are required to maintain lean muscle mass and keep your metabolism going. Additionally, essential amino acids are crucial for healthy immune system function and wound healing.
Researchers at Arizona State University and the Mayo Clinic in Arizona investigated the role of essential amino acids for patients recovering from bariatric surgery. (4) Researchers analyzed the potential impact of essential amino acids, particularly leucine, on recovery and muscle synthesis after surgery. It was concluded that essential amino acid supplements have important implications for maintaining lean muscle tissue and improving patients’ health status following bariatric surgery. (4)
It is important to consume high-quality protein sources that offer ideal amounts of all essential amino acids to ensure that you don’t suffer a protein deficiency post-surgery. There are many high-quality protein sources of varying textures, depending on where you are in the recovery process. High-quality proteins that offer optimal ratios of essential amino acids include milk, low-sugar yogurt, soy milk, low-fat mozzarella cheese, cottage cheese, tofu, fish, lean meats, and eggs. Plant-based protein sources contain essential amino acids but must be combined throughout the day to get a balanced ratio of all essential amino acids. Good options for plant-based protein following bariatric surgery include lentils, black beans, chickpeas, flaxseeds, chia seeds, quinoa, brown rice, oatmeal, walnuts, and pecans.
Whey protein powder and essential amino acid supplements are extremely effective for fighting protein deficiency associated with bariatric surgery. Since the amount of food you can eat post-surgery is limited, eating more protein isn’t the answer to protein deficiency. On the other hand, a supplement is able to supply all the essential amino acids in optimal ratios without an increase in food intake. Essential amino acids supplements, in particular, are likely superior to protein powders because they require no digestion. Consuming essential amino acid supplements supplies individual amino acids in their pure form, saving the digestive system added stress.
Additional Tips for a Successful Weight Loss Surgery
Here are a few more helpful tips to help you make a full recovery while supporting your ultimate health goals.
1. Attend Follow-Up Appointments
Make sure to keep up with your doctor and attend all follow-up appointments. Follow-up appointments allow you and your doctor to keep up with your progress, assess any problematic symptoms, and adjust your regimen as needed. Attending follow-up appointments can serve as benchmarks of your successes and help keep you motivated.
2. Keep Portions Small
Following all guidelines for portions sizes is important for allowing your stomach and digestive system to heal. Remember, your body has just experienced a physical injury and must work hard to heal. Overloading the stomach and intestine with large quantities of food strains the surgical site and can lead to stretching, tearing, and internal bleeding.
3. Avoid Foods That May Irritate the Stomach
Certain foods, even if they are liquid or soft, may contain irritants that aggravate the stomach lining. Steer clear of carbonated drinks like club soda and soft drinks. Avoid fruits like oranges, tangerines, grapefruit, and persimmon. (3) These fruits could potentially cause the formation of phytobezoars, which are clumps of plant materials that cannot be broken down and get caught in the digestive system, potentially causing complications. (3) Avoid spicy foods like hot sauce that could contribute to uncomfortable complications like heartburn.
4. Physical Activity
Adding physical activity into your routine, once you’ve been cleared by a physician, will be vital to maintaining your weight loss while supporting your overall health. Physical activity is crucial for maintaining muscle mass and supporting a healthy metabolism, heart function, blood pressure, and insulin function. Try starting out by walking a few minutes each day, and gradually increase your exercise level to incorporate both aerobic training and strength training. Consistent exercise also has important repercussions for mood and motivation and may help you get even better results from your weight loss surgery.
5. Take Care of Your Mental Health
Weight loss surgery is certainly a physical challenge, but it is also an emotional challenge. Undergoing a weight loss procedure requires you to make significant changes to your daily life, which can be very unsettling and frightening at first. When making significant changes, it is crucial to have the support of a mental health counselor to ensure that the changes you make are sustainable and done in a healthy way. A counselor can also help you address any underlying stressors you may be dealing with that are impacting your daily life.
A mental health counselor is an important resource both before and after surgery. He or she can help with strategies for handling disordered eating patterns, re-establishing a healthy relationship with food, and employing coping mechanisms for stress.
6. Surround Yourself with Support
Undergoing bariatric surgery is a tough process that not only challenges you physically but also mentally and emotionally. Surround yourself with people who are willing to hold you accountable, support your goals, and lift you up when needed. Reach out for help from trusted friends and family members when you need it, and don’t be afraid to cut people out who sabotage your goals.
Additionally, support groups can be a great resource for support and motivation. Chances are, many other people in your area have undergone weight loss surgery and are on the same recovery road as you are.
Other Kinds of Weight Loss Procedures
The weight loss balloon is a less common weight loss procedure that doesn’t require surgery. Instead, a balloon filled with saline is inserted through the mouth into the stomach, where it takes up space and creates the sensation of a full stomach.
Another procedure called adjustable gastric banding involves laparoscopically placing a band around a portion of the stomach. The gastric band can be tightened and helps facilitate weight loss by inhibiting the rapid flow of food from the stomach into the intestine. Food particles spend more time in the stomach and send more signals to your brain that you are feeling full. As a result, you will be inclined to eat less, and your body will take in fewer calories.
How to Choose the Best Weight Loss Surgery for You
When it comes to weight loss surgery, your physician will be able to evaluate which form of surgery works best for your BMI and health conditions.
Conclusion
The ultimate goal of any kind of bariatric surgery is to help you reach a healthy weight, reverse metabolic conditions, and increase your quality of life. Though weight loss surgery should be a last resort, it is an extremely effective treatment for obesity and associated conditions, like fatty liver disease. Following diet and lifestyle patterns that support weight loss surgery are critical for ultimate long-term success.
References:
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4888907/
(2) https://www.ncbi.nlm.nih.gov/pubmed/25802066