Fatty liver disease is a common condition that affects millions of Americans and is often connected to metabolic dysfunction. The progression of fatty liver disease can lead to fibrosis of the liver and other serious liver diseases. Thankfully, there are supplements, diet changes, and lifestyle changes that can facilitate the reduction of liver fat and prevent further damage.
Can you live without a liver? It’s impossible to live without a liver, which is why it’s so important to protect this vital organ. Read on to find out how you can manage fatty liver disease and prevent progression to liver fibrosis.
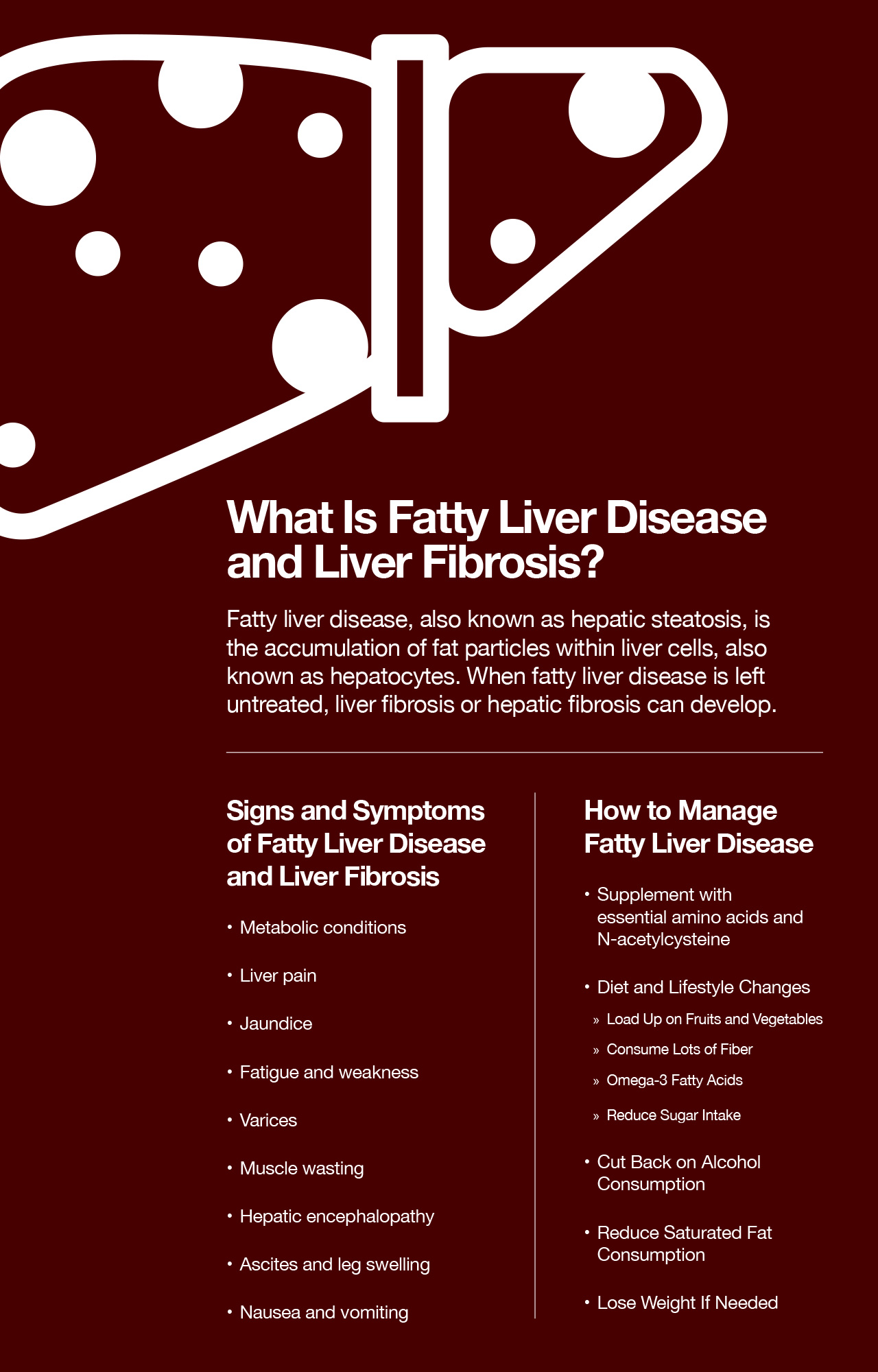
What Is Fatty Liver Disease and Liver Fibrosis?
Fatty liver disease, also known as hepatic steatosis, describes the accumulation of fat particles within liver cells, also known as hepatocytes.
Over time, chronic fatty liver disease results in liver inflammation associated with nonalcoholic steatohepatitis (NASH). When fatty liver disease is left untreated, liver fibrosis or hepatic fibrosis can develop. When fibrotic processes occur in the liver, this means that liver tissue has been injured. Collagen and other fibrous tissue begin to build up around hepatocytes in the extracellular matrix, forming scars.
What happens if liver fibrosis is left untreated? If fibrotic mechanisms continue within the liver without intervention, a significant amount of scar tissue begins to develop, and advanced fibrosis may lead to liver cirrhosis. When an individual has liver cirrhosis, soft liver tissue begins to harden and lose function.
Untreated liver cirrhosis increases the risk of developing hepatocellular carcinoma, or liver cancer. Chronic liver disease in the form of cirrhosis also increases the risk of liver failure. Other complications may also arise, including portal hypertension and biliary cholangitis.
What Are the Causes of Fatty Liver Disease and Fibrosis?
There are numerous underlying conditions and factors that contribute to the development of fatty liver disease and liver fibrosis.
- High-fat, high-sugar diet and sedentary lifestyle: An unhealthy diet and lifestyle are common causes of fatty liver disease. Consuming lots of saturated fat and added sugar while getting insufficient levels of physical activity contributes to liver inflammation and fatty liver disease. Saturated fat and added sugars both contribute to metabolic dysfunction and weight gain, leading to fat deposits in the liver. This form of fatty liver disease is referred to as nonalcoholic fatty liver disease (NAFLD).
- Alcohol consumption: Excess alcohol consumption over time can negatively impact the liver. The liver is responsible for detoxifying and processing alcohol. Chronic and excessive alcohol consumption increases oxidative stress in the liver and results in fatty deposits, causing alcoholic fatty liver disease.
- Viral hepatitis: Chronic viral hepatitis results in ongoing infection and subsequent damage. Hepatitis A, hepatitis B, and hepatitis C are possible viral infections that can cause fatty liver disease.
- Autoimmune hepatitis: Autoimmune hepatitis describes a condition in which the immune system mistakes the liver as harmful tissue. The immune system then launches a misguided attack against healthy liver tissues, resulting in liver damage.
- Hemochromatosis: Hemochromatosis is a genetic condition in which the body doesn’t properly process iron. As a result, excess iron accumulates throughout the body, including the liver. Iron deposits in the liver can impair liver function and result in fatty liver disease and liver fibrosis.
Diagnosis of Liver Disease
There are a number of strategies that physicians use to diagnose fatty liver disease. Abnormalities on routine blood tests are usually a first indicator that the liver isn’t functioning as it should. Individuals with fatty liver disease often have high enzyme levels, indicating inflammation.
If a physician suspects that you have fatty liver disease, you may undergo further testing. Imaging tests like ultrasounds and magnetic resonance imaging (MRI) are noninvasive diagnostic strategies that can reveal the fat content of the liver as well as any liver lesions or scarring. Medical imaging can also reveal an enlarged liver, indicating inflammation as a result of liver disease. Liver elastography tests specifically evaluate liver tissue stiffness. More liver stiffness indicates the accumulation of scar tissue consistent with liver fibrosis.
A liver biopsy may also be performed, to evaluate the presence of liver injury and the fat content of liver tissue.
Signs and Symptoms of Fatty Liver Disease and Liver Fibrosis
In the early stages, fatty liver disease may present no symptoms. However, as liver disease progresses, there are a number of symptoms as liver function becomes increasingly impaired.
- Metabolic conditions: Metabolic conditions like type 2 diabetes, insulin resistance, and obesity are often associated with NAFLD and are risk factors for developing fatty liver disease.
- Liver pain: If you have fatty liver disease or liver fibrosis, you may experience pain in the liver. Liver pain location includes the upper right quadrant of the abdomen.
- Jaundice: Jaundice refers to the yellowing of the skin and whites of the eyes. Jaundice occurs as a result of impaired liver function and bilirubin build-up.
- Fatigue and weakness: The liver is a vital organ that is required to process and detoxify all substances in the body, allowing biological processes to progress normally. When the liver isn’t doing its job, your energy levels may be affected and you may experience more fatigue and weakness.
- Varices: Varices is a condition that describes bulging veins as a result of blocked blood flow somewhere else in the body. Esophageal varices commonly accompanies liver cirrhosis.
- Muscle wasting: Low muscle mass percentages are a common sign of advanced liver disease like liver cirrhosis.
- Hepatic encephalopathy: Hepatic encephalopathy is a complication that occurs in late-stage liver disease. When the liver has lost a significant amount of its function, toxins and other harmful substances accumulate in the bloodstream.
- Ascites and leg swelling: Liver disease inflicts pressure on the portal vein that impairs the flow of blood and fluids throughout the body. As a result, fluid may accumulate in the abdomen and the legs, causing significant swelling.
- Nausea and vomiting: The liver is linked to the digestive system, and nausea and vomiting commonly accompany liver disease.
Treating Liver Disease
In order to prevent liver damage, it’s important to treat and resolve the underlying cause that’s creating the damage. For example, if you have hepatitis C virus (HCV) and chronic hepatitis C infection, your healthcare provider will likely prescribe antiviral medications to clear the infection.
In serious cases in which liver disease progresses to end stage liver disease, liver transplantation may be required. A liver transplantation replaces damaged liver tissue with healthy liver tissue from a donor.
How to Manage Fatty Liver Disease
When caught early, fatty liver disease is highly manageable and reversible. Diet and lifestyle changes are crucial for managing fatty liver disease and preventing liver fibrosis. Here are some helpful strategies and tips for managing fatty liver disease at home.
Supplements
Research shows that essential amino acids and N-acetylcysteine play a crucial role in supporting a healthy liver.
Essential Amino Acids Supplements
Essential amino acids are building blocks of protein that the body requires to carry out all biological processes successfully. Taking essential amino acid supplements has been scientifically shown to improve liver fat levels. In a study published in Nutrition, researchers evaluated the effect of taking essential amino acids and arginine in 12 elderly individuals. (1) Results revealed that taking the amino acid blend was connected to a drop in plasma triglyceride levels as well as a decrease in liver fat. (1)
Additionally, it is also helpful to make sure that you’re getting high-quality protein in your daily diet. High-quality protein sources include chicken breast, turkey breast, fish, nonfat yogurt, and skim milk. All animal proteins offer optimal ratios of essential amino acids.
On the other hand, it’s necessary to combine vegetable proteins throughout the day to obtain optimal ratios of essential amino acids from plant-based sources. Whole grains, nuts, seeds, beans, and soy products are great sources of plant protein.
N-Acetylcysteine
N-Acetylcysteine (or NAC) functions as an antioxidant in the body and has been connected to anti-aging properties and mitochondrial health. In addition, NAC may be helpful for supporting liver function in individuals with nonalcoholic fatty liver disease. In a study published in Hepatitis Monthly: International Monthly Journal in the Field of Hepatology, researchers found that taking NAC was connected with lower levels of alanine aminotransferase. (2)
The raw materials that the body uses to manufacture NAC can be found in a number of foods like chicken, lentils, tuna, and garlic. While these foods can offer building blocks, it may also be a good idea to take high-quality supplements that offer NAC, to make sure that you’re getting enough NAC on a daily basis.
Diet and Lifestyle Changes
There are steps you can take to support healthy diet and lifestyle changes that fight against fatty liver disease.
1. Load Up on Fruits and Vegetables
Fruits and vegetables are an important part of a liver-friendly diet that fights against fatty liver disease and helps prevent progression to fibrosis and cirrhosis. Fruits and vegetables are packed with antioxidants and anti-inflammatory components that help repair damaged tissues and reduce inflammation in liver cells. Examples of healing elements in fruits and veggies include polyphenols, carotenoids, and vitamin C. Fruits and veggies to incorporate into a liver-friendly diet include apples, blueberries, strawberries, papaya, mango, spinach, kale, and broccoli.
2. Consume Lots of Fiber
Gut health is linked to liver health. If you have fatty liver disease or liver fibrosis, consuming enough dietary fiber is part of a liver-friendly diet. When we eat dietary fiber, the good bacteria in the digestive tract flourish and feed on fiber particles and produce anti-inflammatory components as byproducts.
These compounds then travel throughout the body and help to reduce inflammation in different organ systems, including the liver.
3. Omega-3 Fatty Acids
Omega-3 fatty acids are healthy polyunsaturated fats that have potent anti-inflammatory effects on the body, including the liver. You can obtain omega-3 fatty acids from fish like salmon, mackerel, sardines, and Arctic char. Chia seeds, flaxseeds, walnuts, and pecans also provide a plant form of omega-3 fatty acids called alpha-linolenic acid (ALA).
4. Reducing Sugar Intake
It seems like sugar is added to everything these days; from desserts to salad dressings, sugar always seems to be an ingredient. The high intake of added sugar in the American diet is a significant factor driving high rates of type 2 diabetes, insulin resistance, obesity, and fatty liver disease. When we eat foods with added sugar, the digestive system quickly breaks down the sugar into glucose molecules. Glucose immediately enters the bloodstream and causes major blood sugar spikes. These sugar spikes provide a burst of short-lived energy, and unused glucose is then deposited as fat throughout the body.
Cutting back on added sugar consumption can improve liver health and help reduce the fat content of your liver. Avoiding foods like cakes, cookies, ice cream, candy, soda, and sugar-laden condiments help stabilize blood sugar levels, lower inflammation, and reduce fat deposits.
In addition, it’s important to also stay away from refined grains, which tend to have the same impact on metabolism as added sugars. Steer clear of foods like white bread, white rice, and white pasta.
5. Cutting Back on Alcohol Consumption
Alcohol consumption is the major factor contributing to alcoholic fatty liver disease. Alcohol, especially when consumed in large quantities, causes inflammation and oxidative damage, particularly in the liver. Consuming alcohol in excess causes fat accumulation, resulting in alcoholic fatty liver disease. Over time, continued alcohol consumption can cause scar formation in the liver, causing liver fibrosis and liver cirrhosis.
The best way to halt the progression of alcoholic fatty liver disease is to stop drinking. Dramatically reducing your alcohol consumption allows your liver to heal from inflammation and damage and prevent further progression of disease. If you struggle with alcohol abuse or addiction, it’s best to connect with a mental health provider and a support group to find a strategy that works best to help you cut back on drinking.
6. Reduce Saturated Fat Consumption
Like added sugar, saturated fat is connected to noncommunicable conditions like type 2 diabetes, insulin resistance, obesity, and fatty liver disease.
Saturated fat is found in fatty meat and dairy products, such as steak, bacon, whole milk, cream, and butter. Eating too much saturated fat interferes with insulin function, drives up cholesterol and triglyceride levels, and contributes to weight gain. Moreover, a high saturated fat intake over time significantly increases the risk of cardiovascular disease.
7. Losing Weight If Needed
Weight loss alone can have a significant positive impact on fatty liver disease. As the body loses fat deposits, the fat content of the liver will also naturally decrease.
You can encourage fat loss by creating a moderate calorie deficit in your daily diet. This means you should consume fewer calories than you burn. However, avoid undereating – a counterproductive and unsustainable strategy that leads to metabolic damage and rebound weight gain.
To encourage weight loss, strive to eat a healthy, balanced diet and engage in regular physical activity.
Things to Keep in Mind
If you have been diagnosed with a liver condition like fatty liver disease or liver fibrosis, it is crucial to make diet and lifestyle changes under the supervision of your physician. Always check with your doctor before making any drastic diet or lifestyle changes or before starting new supplements.
How to Manage Fatty Liver Disease and Prevent Liver Fibrosis: Conclusion
Fatty liver disease describes the accumulation of fat particles within liver cells. When left untreated, fatty liver disease can progress to NASH, liver fibrosis, and liver cirrhosis. Diet and lifestyle changes can help reverse damage and prevent further damage to the liver. Essential amino acid and NAC supplementation combined with a healthy diet and lifestyle can help reduce liver fat levels and support overall health and well-being.
References:























