The liver is one of the most essential organs in the body and plays a crucial role in detoxifying substances, synthesizing proteins, and producing digestive substances. Though the liver is a vital and resilient organ, it is still possible to develop liver disease. In this article, we discuss the different kinds of liver disease you may develop, possible risk factors, and the early signs of liver disease.
Catching liver disease early is key for intervening and reversing the condition. Read on to find out more!
Early Signs of Liver Disease May Be Difficult to Detect
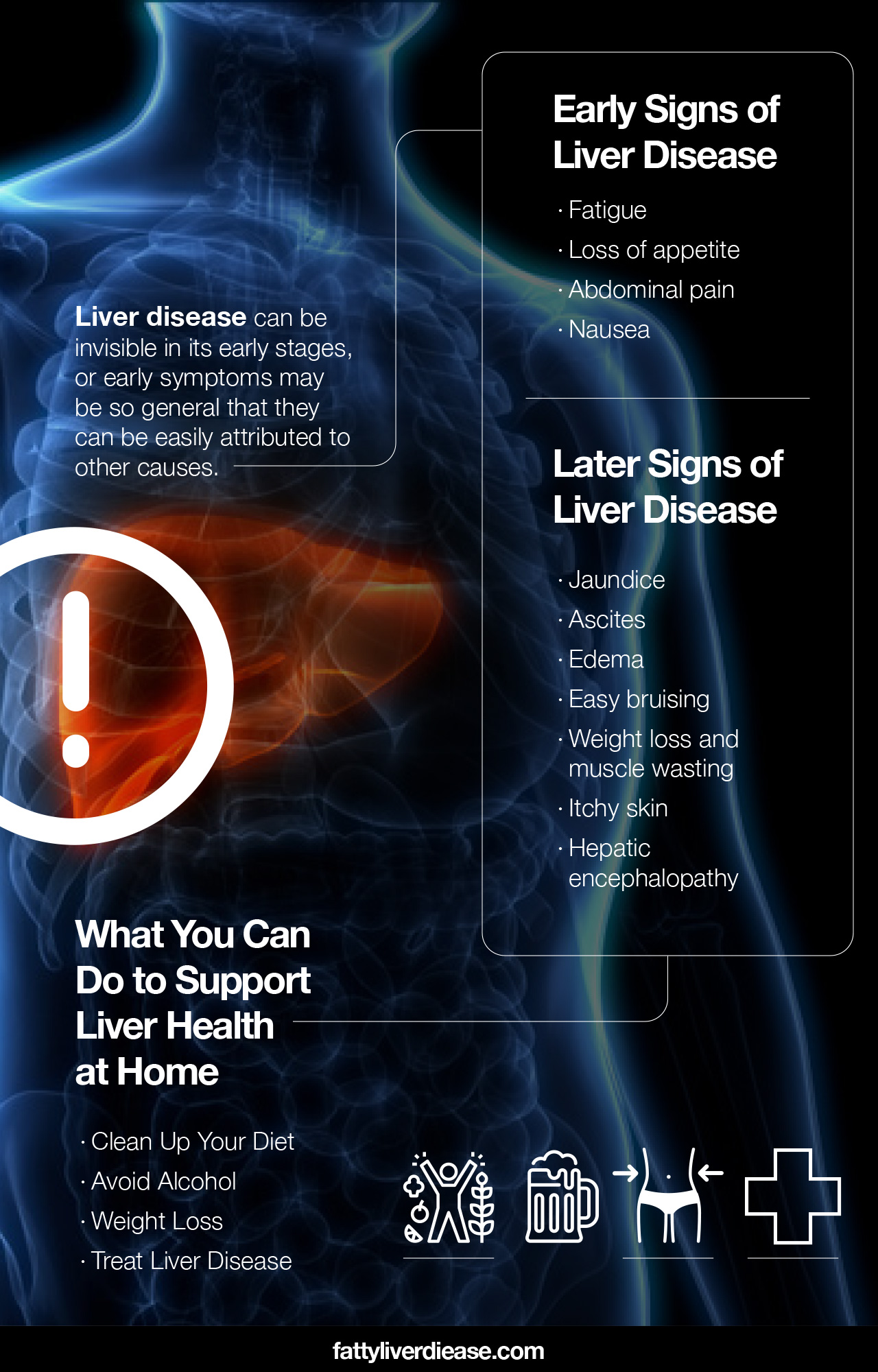
The early stages of liver disease may not exhibit any symptoms. Or, early symptoms may be so general that they can be easily attributed to other causes. Because liver disease can be invisible in its early stages, it’s important to stay vigilant with attending doctor’s appointments and yearly check-ups. Here are a few examples of early liver disease symptoms.
- Fatigue: Fatigue is one of the most common early signs of liver disease. However, fatigue can be attributed to many different conditions.
- Loss of appetite: If you have liver disease, you may experience a loss of appetite.
- Abdominal pain: Abdominal pain may appear in the early stages of liver disease. In particular, you may feel abdominal pain in the upper right side of your midsection. This is where the liver is located, making it the primary liver pain area.
- Nausea: Nausea may go hand-in-hand with loss of appetite, as liver disease can have an impact on gastrointestinal health.
Later Signs of Liver Disease
As liver disease progresses, symptoms become more exaggerated and apparent. Here are some warning signs and symptoms of liver disease and signs of liver damage.
- Jaundice: Jaundice describes the yellowing of the skin with more progressed forms of liver disease due to accumulated bilirubin in the bloodstream. If you have jaundice, you will likely notice a yellow hue in your skin and whites of the eyes.
- Ascites: Ascites describes the accumulation of fluid in the abdomen. Ascites is characterized by apparent bloating and enlargement of the abdomen.
- Edema: Edema or swelling in the lower extremities is common with advanced forms of liver disease. Liver damage can impact the portal vein and impede the normal blood flow through the veins, causing blood and fluid to accumulate in the legs and feet.
- Easy bruising: Easy bruising is common in progressed forms of liver disease. When liver function is compromised, the liver does not produce sufficient amounts of clotting proteins. As a result, the body is sensitive to even minimal impacts.
- Weight loss and muscle wasting: Weight loss and muscle wasting are common symptoms associated with later stages of liver disease. When the liver cannot function normally, it cannot properly process foods into energy and components needed for muscle synthesis. You may notice that you lose weight unintentionally and become weaker.
- Itchy skin: Persistently itchy skin is also common with later stages of liver disease that affect the biliary ducts and gallbladder. Itchiness arises from bile products accumulating beneath the skin, motivating the urge to scratch.
- Hepatic encephalopathy: Hepatic encephalopathy is a symptom of advanced liver disease that affects mental functioning. When the liver cannot detoxify harmful compounds in the body sufficiently, these compounds build up in the bloodstream and travel to all organs. In the case of hepatic encephalopathy, ammonia is the primary culprit that interferes with normal brain function. Symptoms of hepatic encephalopathy include confusion, anxiety, and seizures.
Risk Factors for Developing Liver Diseases
Knowing whether you are at risk for developing liver disease is important information for both you and your doctor. Here are a few factors that are correlated with a higher risk of liver disease.
Eating a Diet High in Sugar and Fat
Eating lots of added sugars, refined grains, and saturated fat is a recipe for metabolic dysfunction and fatty liver disease. High consumption of added sugars and refined grains causes blood sugar levels to increase dramatically. The pancreas must then release the hormone insulin to communicate to the body’s cells to utilize the glucose present in the bloodstream for energy. However, chronic consumption of excess sugar can cause insulin to malfunction, leading to metabolic conditions like insulin resistance, type 2 diabetes, and fatty liver disease.
Many people know about the association between saturated fat and heart disease. However, a high intake of saturated fat also negatively impacts insulin and metabolic functions. Eating too much saturated fat from meat and cheese can contribute to weight gain and metabolic conditions like insulin resistance and fatty liver disease.
Being Overweight
Carrying around too many extra pounds can increase your risk of developing fatty liver disease. Obesity is often a sign of an unhealthy diet, a dysfunctional metabolism, hormonal imbalances, or all of these factors. Excess fat deposits throughout the body may also be associated with fat deposits in the liver.
Chronic Alcohol Abuse
Chronic alcohol abuse is defined by drinking more than the recommended number of drinks on a daily basis. Constantly drinking puts pressure on the liver that can ultimately lead to alcoholic fatty liver disease, steatohepatitis, liver cirrhosis, and other alcohol-related liver diseases. Heavy drinkers tend to be at a higher risk of developing liver disease.
Chronic alcohol use puts an immense amount of stress on the liver and causes oxidative stress. Chronic consumption of alcohol doesn’t allow the body time to heal from the oxidative stress. As a result, free radicals accumulate within the liver, cause damage, fat accumulation, scarring, and subsequent hepatic impairment.
Binge Drinking
Usually, chronic alcohol consumption is linked to liver disease. However, it’s important to know that binge drinking may actually increase the risk of developing liver disease, though it is often regarded as a social norm. Researchers in Finland examined 6366 subjects for binge drinking habits and hospital admissions for liver issues. (1) Results found that individuals engaging in binge drinking behavior were more likely to develop liver disease, especially when metabolic syndrome was a comorbid condition. (1)
Binge drinking involves consuming excessive amounts of alcohol on one occasion. When an individual engages in binge drinking, the liver becomes inundated with alcohol to metabolize and detoxify. This can cause significant oxidative stress within the liver that the body must work hard to make up for. It’s important to note that after binge drinking, liver enzymes are elevated, and the body must recover from excess alcohol consumption.
Family History of Liver Disease
If your parents or other family members have had liver conditions, you may be at a higher risk of developing liver disease. Genetics can influence many factors that contribute to liver disease, such as metabolic mechanisms, liver biochemistry, and immune system function.
Types of Liver Diseases
Let’s go over the different kinds of liver diseases. Though the most commonly seen liver diseases in the United States are nonalcoholic fatty liver disease, alcohol-related liver disease, and hepatitis C, there are also other liver diseases.
- Nonalcoholic fatty liver disease: Nonalcoholic fatty liver disease is one of the most common liver diseases in the United States. Nonalcoholic fatty liver disease is characterized by the buildup of fat particles within liver cells. As described above, this form of fatty liver disease is connected primarily to metabolic dysfunction, obesity, and a diet high in refined grains, added sugar, and saturated fat.
- Alcoholic fatty liver disease: Alcoholic fatty liver disease is also characterized by fat accumulation within liver cells. However, the causal factor for alcoholic fatty liver disease is excess alcohol consumption.
- Viral hepatitis: Possible viral infections include hepatitis A, hepatitis B, and hepatitis C. Infection with certain viruses causes liver inflammation that over time leads to more serious liver conditions like cirrhosis.
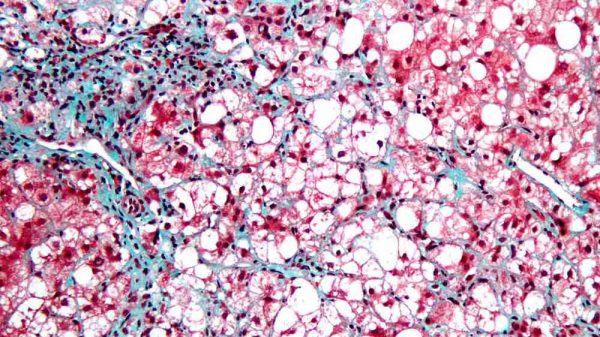
- Liver fibrosis: Liver fibrosis describes a process in which collagen-like material accumulates around liver cells. Continued inflammation in the liver from conditions like nonalcoholic fatty liver disease, alcoholic fatty liver disease, and hepatitis can cause fibrosis to occur. Over time, without intervention, fibrosis causes significant scarring in the liver.
- Liver cirrhosis: Continued fibrosis causes cirrhosis of the liver, which is the buildup of scar tissue. Liver cirrhosis causes healthy liver tissue to harden and lose its ability to carry out normal functions. Cirrhosis, without medical intervention, can lead to seriously compromised liver function, end stage liver disease, and liver failure.
- Autoimmune hepatitis: Autoimmune hepatitis is a condition resulting from a malfunctioning immune system. A healthy immune system is able to identify harmful cells and infections resulting from viruses and bacteria. A healthy immune system is also able to distinguish between healthy tissue and harmful cells. In the case of autoimmune hepatitis, the immune system identifies a healthy liver as harmful and launches a misguided attack on the liver. The liver then becomes inflamed, and over time, liver function deteriorates.
- Liver cancer: Liver cancer, or hepatocellular carcinoma, is characterized by the development of malignant growths within the liver.
What to Do If You Suspect Liver Disease
If you think you may be suffering from liver problems, it’s critical to make an appointment with your doctor as soon as possible. Your healthcare provider will be able to assess your symptoms, liver health, and provide medical advice and recommend the best treatment options.
So, how exactly will your physician evaluate your liver health? First, he or she will listen to your symptoms. Your doctor will also identify if you are at risk of developing a liver disease based on your family history, diet, drinking habits, and metabolic health. Your physician may be able to tell if the liver is enlarged or inflamed based on a physical examination.
If liver disease is suspected, your general practitioner will refer you to other radiology and hepatology experts to further evaluate your liver health. Radiologists will conduct imaging tests that reveal further information about your liver. Ultrasounds, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans can show abnormalities present in the liver, such as growths, fat accumulation, and scar tissue.
What You Can Do to Support Liver Health at Home
There are three critical steps you can take to support your liver health at home.
1. Clean Up Your Diet
Eating healthy foods and avoiding junk foods is important for improving your liver health. As discussed above, steer clear of refined grains, added sugars, and saturated fats, which cause metabolic dysfunction. Consume an abundance of foods that offer antioxidants, vitamins, minerals, complex carbs, healthy fats, fiber, and optimal ratios of essential amino acids.
Fruits and vegetables are packed with micronutrients like vitamins, minerals, and antioxidants that help reverse oxidative damage. Whole grains and beans are packed with fiber to support gut health and lower systemic inflammation. Nuts, seeds, and fatty fish offer omega-3 fatty acids, which exhibit potent anti-inflammatory activity in the liver. Fish, lean meats, and low-fat dairy offer high-quality protein with optimal ratios of essential amino acids, which can fight against muscle wasting and support healthy liver mechanisms.
2. Avoid Alcohol
Cutting alcohol out of your lifestyle is a key step in protecting your liver health. Whether you have nonalcoholic fatty liver disease, alcoholic liver disease, alcoholic cirrhosis, alcoholic hepatitis, or viral hepatitis, drinking alcohol only worsens your liver condition. The liver is a highly adaptable organ and is able to regenerate. So, avoiding alcohol gives your body the opportunity to heal from alcohol-induced oxidative stress and inflammation.
If you think you may be physically dependent on alcohol, seek medical advice from a health professional regarding the best way to detox from alcohol. There are numerous inpatient and outpatient treatment programs designed to support individuals struggling with alcohol addiction. It’s also a good idea to speak to a licensed addiction specialist who can recommend treatment programs in your area.
3. Weight Loss
When necessary, losing weight can help regulate metabolic functions, lower systemic inflammation, and balance hormones. If you are striving to lose weight, focus on eating healthy foods, monitoring calorie intake, and engaging in regular physical activity. Weight loss is beneficial for reversing fat accumulation in the liver.
Treating Liver Disease
Can liver damage be reversed? Depending on the type of liver disease and the extent of damage, liver damage can be reversed. In some cases, diet and lifestyle changes may be sufficient for treatment. However, in other cases, other medications and treatments are effective. For example, hepatitis C can be treated with antiviral medications, and autoimmune hepatitis can be managed with immunosuppressant drugs.
In very advanced forms of liver disease in which the liver has lost the majority of its function, the damage is likely beyond repair. Can you live without a liver? It’s impossible to live without a liver. A liver transplant is the most effective form of treatment for individuals with end stage liver disease and liver failure.
Early Signs of Liver Disease: Conclusion
A healthy liver is vital for overall health and wellness. Early signs of liver disease may not be present at all, or they are very generalized symptoms, such as fatigue and abdominal pain. Catching liver disease early is important for the best outcome possible. In some cases of liver disease, especially nonalcoholic fatty liver disease, the condition can be reversed completely with diet and lifestyle changes. If you think you may be at risk for developing liver disease or you are noticing warning signs and symptoms, it’s important to talk to your doctor as soon as possible.
References: