You might have just received a diagnosis of diffuse hepatic steatosis. You might be confused and be wondering what it means to have diffuse hepatic steatosis. If your physician has informed you that you have diffuse hepatic steatosis, don’t panic. In many cases, diffuse hepatic steatosis is indicative of a liver condition that can be treated.
Read on to find out everything you need to know about diffuse hepatic steatosis.
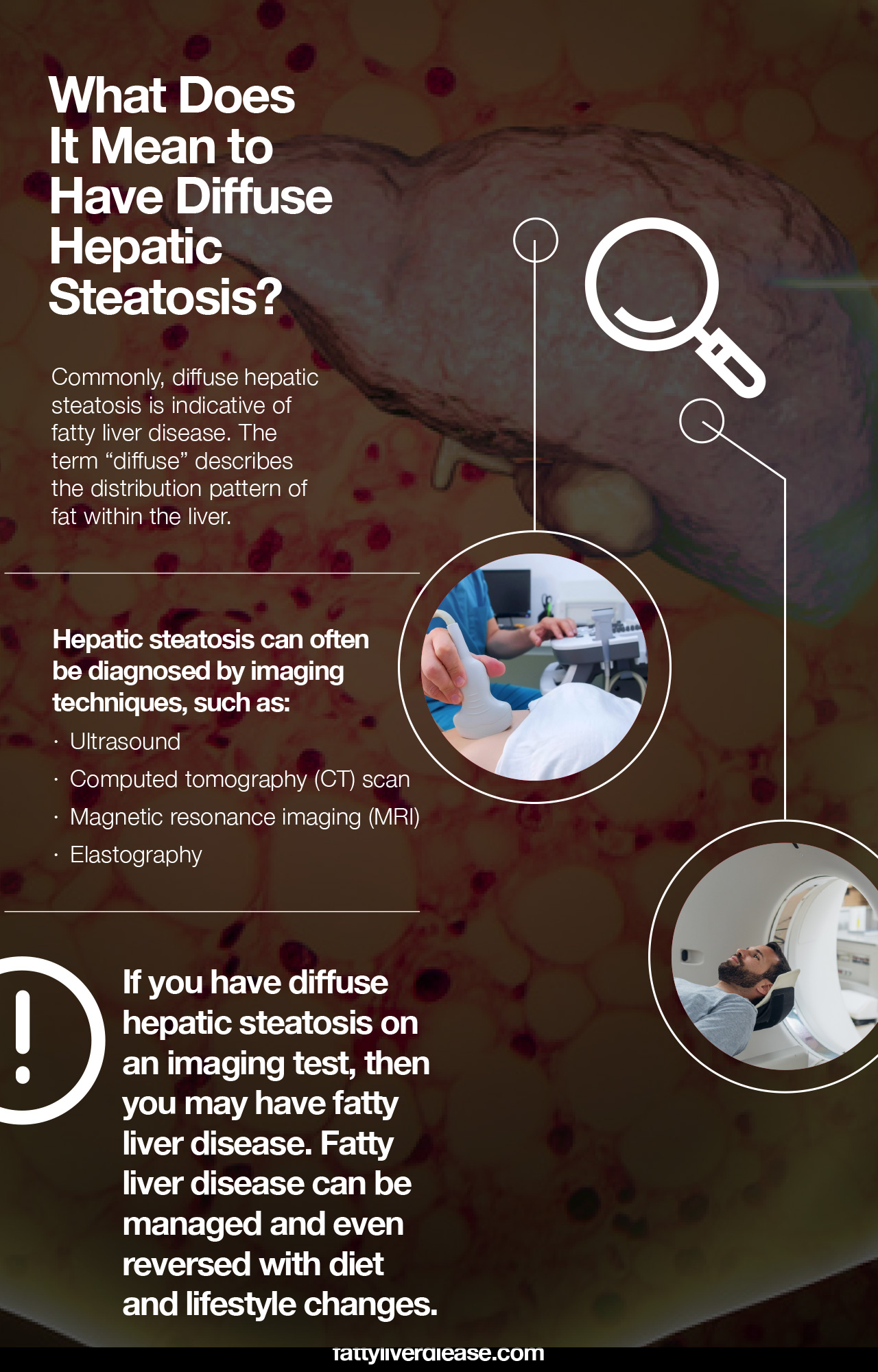
What Does It Mean to Have Diffuse Hepatic Steatosis?
If you have been told that you have diffuse hepatic steatosis, this indicates that you have fatty infiltration of the liver. The term “diffuse” describes the distribution pattern of fat within the liver. When fat particles are widely dispersed throughout the liver, this finding is called diffuse hepatic steatosis. Diffuse hepatic steatosis differs from focal fatty deposits, which occur in localized areas within the liver. Hepatic steatosis is the medical term that describes the accumulation of fat or lipids within liver cells, or hepatocytes.
Commonly, diffuse hepatic steatosis is indicative of fatty liver disease. Fatty liver disease means that you have excess fatty acids in your liver. Medically, your liver must be at least 5% fat to meet the criteria for a diagnosis of fatty liver disease. Fatty liver disease can be classified as either nonalcoholic or alcoholic.
Nonalcoholic fatty liver disease – also called hepatic steatosis or hepatosteatosis- most often occurs due to diet and lifestyle factors, while alcoholic fatty liver disease is fueled primarily by alcohol intake. Nonalcoholic fatty liver disease is associated with conditions like metabolic syndrome, obesity, and hypertension. Genetic factors most likely contribute to the development of both nonalcoholic and alcoholic fatty liver disease as well. Fatty liver disease has a very high prevalence rate across the general population in the United States.
What Does Diagnosis Look Like?
Hepatic steatosis can often be diagnosed by imaging techniques, such as ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI). All types of medical imaging can reveal diffuse fat content in the liver. This finding may also be described as lower liver attenuation, which means that healthy tissue is interrupted by fatty deposits. Imaging tests are performed by radiology specialists and interpreted by radiologists.
Ultrasound imaging is a type of sonography that is useful for detecting fat within the liver. Ultrasound technology utilizes sound waves to detect variations in structures and composition within body tissues. A higher measure of echogenicity will also accompany fat deposits in the liver parenchyma, which is the part of the liver responsible for carrying out the organ’s processes. Higher echogenicity means that sound waves more readily bounce off fat tissue and “echo” back to their source. An MRI might reveal a chemical shift that signifies the presence of fat within the liver.
Another type of imaging is called elastography. Elastography can reveal if soft tissue has hardened, indicating damage. For example, normally functioning liver tissue is soft in texture. Scarred or damaged liver becomes harder in texture.
Other tests can also reveal information about liver function as well as the presence of fat in the liver. Your physician may administer a blood test to examine the levels of liver enzymes present in the blood, particularly aspartate transaminase (AST), alanine transaminase (ALT), and gamma-glutamyl transpeptidase (GGT). Elevated levels of these enzymes indicate liver inflammation that is consistent with fatty liver disease.
In some cases, fatty liver disease may also cause an enlarged liver as a result of inflammation. Abnormal liver size may be detected through imaging methods. However, a physician may also be able to see whether you have an enlarged liver or normal liver size through a physical examination.
One of the most definitive ways to detect and diagnose fatty liver disease is through a liver biopsy. A liver biopsy requires taking a tiny sample of your liver and analyzing it for the presence of fat cells, lesions, and other abnormalities.
Your physician will perform an assessment of hepatic steatosis in your particular case and give you treatment recommendations. Internists, as well as specialists in gastroenterology and hepatology, may treat fatty liver disease. After an initial diagnosis, you will receive treatment recommendations and may be asked to make follow-up appointments for further monitoring.
Signs and Symptoms of Nonalcoholic Fatty Liver Disease
Initially, nonalcoholic fatty liver disease (also referred to as NAFLD) may have no symptoms at all. However, as the condition progresses, it may start to exhibit symptoms. Here are a few signs and symptoms of fatty liver disease:
- Fatigue
- Feeling weak
- Unexplained weight loss
- Pain in the upper right quadrant of your abdomen
If nonalcoholic liver disease progresses to more serious conditions, it can cause more severe symptoms like ascites, jaundice, muscle wasting, and hepatic encephalopathy.
Keep in mind that fatty liver disease rarely occurs in isolation. Metabolic conditions are significant risk factors for developing fatty liver disease. Metabolic syndrome includes conditions like insulin resistance, type 2 diabetes, elevated triglycerides, and high cholesterol. Fatty liver disease is also correlated with obesity and hypertension.
Progression of Fatty Liver Disease
Fatty liver disease can progress and develop into more severe forms of liver disease. The first step in the progression of fatty liver disease is nonalcoholic steatohepatitis (also referred to as NASH). Steatohepatitis indicates that fatty liver disease is now causing inflammation within your liver. If your liver is inflamed, this means that the liver’s cellular processes are not operating as smoothly as usual. The tissues are irritated, and liver processes are essentially “clogged.”
The progression of liver steatosis tends to be more rapid if you also have other conditions like hepatitis C or iron deposition in the liver.
What is the NASH liver disease life expectancy? Generally, if diet and lifestyle changes are made and recommended medical interventions are followed, an individual with NASH can live a long healthy life.
If NASH is left untreated, it can lead to liver fibrosis, also known as hepatic fibrosis. Fibrosis describes the development of scar tissue in the liver. Over time, fibrosis can lead to liver cirrhosis. Liver cirrhosis describes the significant scarring of the liver and impeded liver functions. Over time, liver cirrhosis can lead to liver cancer or liver failure.
Can Fatty Liver Disease Be Reversed?
Thankfully, fatty liver disease can be reversed with careful lifestyle and diet changes. Here are a few key tips for managing fatty liver disease.
1. Stay Away from Refined Grains and Added Sugar
Refined grain and added sugar are significant contributory components to fatty liver disease and metabolic syndrome. Refined grain and added sugar are quickly broken down into glucose molecules in the digestive system. These glucose molecules then enter the bloodstream and spike blood sugar. Insulin is released and signals to body tissues to utilize the glucose as energy, but inevitably, there is leftover glucose that must be stored throughout the body, including the liver. Eating too many refined carbs and added sugar could, over time, contribute to fatty liver disease as well as metabolic conditions like insulin resistance and type 2 diabetes.
Steer clear of products that contain added sugar, such as candy, soda, pastries, cookies, cakes, and ice cream. Even products like granola bars, breakfast cereals, salad dressing, and condiments can contain more added sugars than you think.
To avoid refined grains, stay away from foods like white rice, white pasta, and white bread. Just like added sugar, refined grains are broken down into glucose.
2. Eat Lots of Fruits and Vegetables
Fruits and veggies are a critical component of the fatty liver disease diet plan. Both fruits and vegetables are chock-full of anti-inflammatory components like polyphenols, carotenoids, and other antioxidants that can fight liver damage. Reach for foods like broccoli, spinach, apples, blueberries, and raspberries for a liver-friendly diet.
3. Avoid Saturated Fat
Like added sugars and refined grains, saturated fat is another culprit implicated in the development of metabolic syndrome and fatty liver disease. Saturated found is present in animal products like full-fat dairy and fatty cuts of meat. Avoid full-fat animal products like milk, yogurt, cheese, bacon, steak, and ground meat. Eating lots of saturated fat over time contributes to insulin dysfunction, fatty liver disease, and weight gain.
4. Lose Weight If Needed
Losing weight can help you reverse fatty liver disease. When you lose fatty tissue, this also means that you are losing fat from your liver.
To facilitate weight loss, aim to create a calorie deficit, meaning you are burning more energy than you consume. Eating healthy foods, controlling portion sizes, and exercising help encourage weight loss.
Make sure that you follow a balanced diet to lose weight, instead of following extreme diet plans. In addition to losing fat, it’s essential to also maintain muscle mass.
5. Eat High-Quality Protein
High-quality protein is crucial because it helps you maintain muscle mass and fortifies the immune system. Protein is vital for all cellular functions and facilitates healing from injury and disease. In particular, protein supplies amino acids, which are indispensable resources for building muscle tissue, neurotransmitters, enzymes, and hormones involved in metabolism. The body requires balanced ratios of essential amino acids on a daily basis. You can get optimal ratios of essential amino acids from healthy animal products like nonfat yogurt, chicken breast, low-fat cheese, and fish.
It’s also possible to the essential amino acids from vegetable protein sources like tofu, whole grains, nuts, seeds, and beans. However, make sure to eat a variety of vegetable proteins throughout the day to ensure that you’re getting the balanced ratios of essential amino acids that you need.
The Fatty Liver Disease Diet Plan
Following a diet plan for fatty liver disease can help you reverse fatty liver disease and prevent fatty liver disease progression to NASH and liver cirrhosis.
How long does it take to reverse fatty liver? The length of time required to reverse fatty liver depends on how progressed your condition is.
For more details about making lifestyle changes for fatty liver disease, check out this article on the fatty liver disease diet plan.
Conclusion: Diffuse Hepatic Steatosis
If you have diffuse hepatic steatosis on an imaging test, then you may have fatty liver disease. Your physician will be able to diagnose fatty liver disease based on physical examination and blood tests. Fatty liver disease can be managed and even reversed with diet and lifestyle changes. However, without treatment, fatty liver disease has the potential to progress to more severe liver conditions if left untreated.