Venous insufficiency is a common condition that affects the veins in the lower legs. Suffering from chronic venous insufficiency can cause uncomfortable symptoms that can progress if left untreated. If you have been diagnosed with venous insufficiency, there are diet and lifestyle changes that you can implement at home to help provide relief for your symptoms.
Read on to find out about how to follow a diet for venous insufficiency as well as other strategies for mitigating your symptoms and improving circulation.
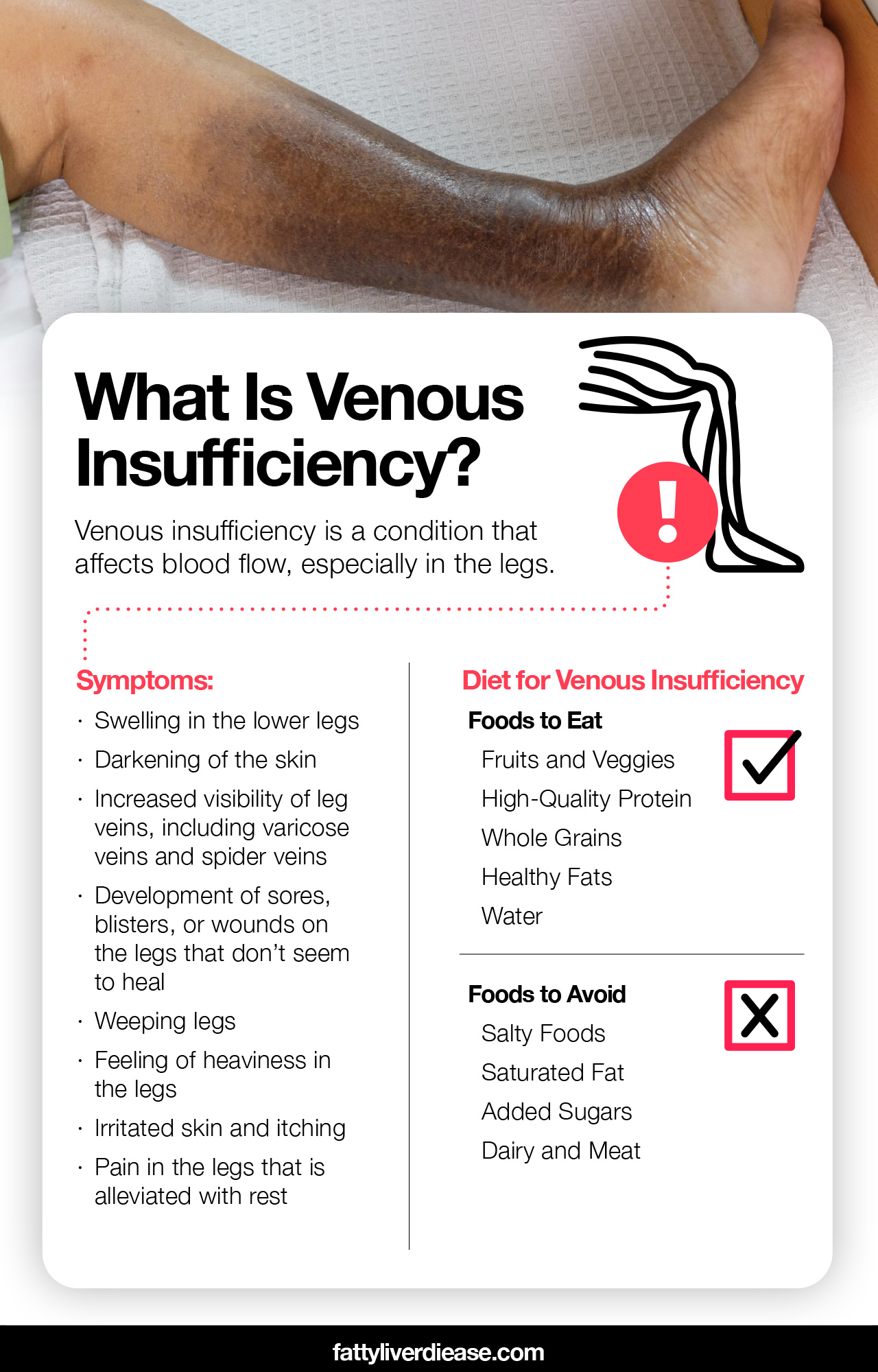
What Is Venous Insufficiency?
Venous insufficiency is a condition that affects blood flow, especially in the legs.
To best understand venous insufficiency, it’s helpful to understand how the circulatory system works. When the heart beats, it pushes oxygen-rich blood throughout the body via blood vessels called arteries. The blood must then return to the heart via a different network of blood vessels, called veins. To facilitate the movement of blood back towards the heart, valves in the veins encourage blood flow against the flow of gravity and back towards your chest.
When these valves aren’t working properly, blood is unable to effectively flow through the veins and back towards the heart. Subsequently, blood collects in the lower limbs and causes swelling.
Stages of Chronic Venous Insufficiency
As is the case with many health conditions, venous insufficiency progresses if left untreated. Research shows that chronic venous insufficiency stages can be categorized by certain clinical and pathophysiological features. (1)
At first, no symptoms will be present. As venous insufficiency persists, early stages may reveal more conspicuous veins and the development of varicose veins. Swelling and changes in pigmentation represent the middle stages of chronic venous insufficiency, while persistent ulcerations are indicative of later stages of the condition.
What Causes Venous Insufficiency?
There are numerous risk factors and causes of venous insufficiency.
- Being overweight: Carrying excess weight puts pressure on the circulatory system and increases systemic inflammation.
- Sedentary lifestyle: Exercising very little can increase venous hypertension and generally weaken the cardiovascular system, leading to worsened blood flow. In fact, remaining sedentary or sitting for long periods of time can limit circulation to the lower legs and increase blood pressure specifically in the lower legs.
- Aging: In combination with being overweight and not exercising, aging is a major risk factor for developing venous insufficiency. As we get older, more wear and tear is placed on the body simply from everyday functioning. The blood vessels tend to be more vulnerable to stress and may become scarred over time, which impacts circulation. Staying active and maintaining a healthy weight can help counteract the effects of aging over time.
- Blood clots: Blood clots are a risk factor for developing venous insufficiency. A blot clot develops when red blood cells stick together and cause a small blockage in the blood vessels. The main type of blood clot that can lead to venous insufficiency is called deep vein thrombosis (DVT), which develops in the lower legs and impedes normal circulation.
- High blood pressure: Having high blood pressure or hypertension is a risk factor for developing venous insufficiency. High blood pressure causes scarring and damage in the vein walls and valves, which decreases circulation.
- Injury or scar tissue: A previous injury or surgery on the legs can inflict damage on the veins in the legs. When venous valves are damaged by scar tissue, they will not work properly and increase your risk of developing venous insufficiency.
- Family history: Having family members with venous insufficiency may indicate a genetic propensity for developing the condition. You may be at a higher risk of developing venous insufficiency.
Symptoms of Chronic Venous Insufficiency
How do you know if you have venous insufficiency? There are numerous symptoms that indicate that you may have venous insufficiency. You may experience symptoms such as:
- Swelling in the lower legs
- Darkening of the skin
- Increased visibility of leg veins, including varicose veins and spider veins
- Development of sores, blisters, or wounds on the legs that don’t seem to heal
- Weeping legs
- Feeling of heaviness in the legs
- Irritated skin and itching
- Pain in the legs that is alleviated with rest
What to Do If You Notice Symptoms
If you observe symptoms that are consistent with venous insufficiency, it is critical to seek medical attention. Determining the underlying cause is necessary to effectively treat venous insufficiency. When you visit the doctor, you will undergo a physical examination and testing to determine a diagnosis. Always follow the treatment recommendations that your doctor provides for you to ensure that you are doing the healthiest thing for your condition.
Diet for Venous Insufficiency: Food to Eat
Maintaining a healthy, anti-inflammatory diet is a critical part of preserving vein health and improving venous insufficiency.
1. Fruits and Veggies
Fruits and vegetables are crucial components of the diet to mitigate venous insufficiency. The vitamins, minerals, and antioxidants in fresh produce have a potent anti-inflammatory effect and help reverse the effects of vein disease. On a molecular level, tiny compounds like flavonoids and vitamin C neutralize damaging free radicals that build up in the vein walls as a result of inflammation. Eating antioxidant-rich foods therefore improves the function of the endothelium, which is a thin layer of muscle tissue that is responsible for dilating and constricting the blood vessels to encourage healthy blood flow.
Overall, eating lots of fruits and vegetables can help improve the function of your veins, allowing blood to circulate more easily through the veins and even reducing blood pressure.
Examples of excellent fruits and veggies to incorporate into your diet include blueberries, blackberries, bell peppers, spinach, broccoli, avocado, and citrus fruits.
2. High-Quality Protein
Research reveals that being deficient in protein is correlated with slow wound-healing time for leg ulcers induced by venous insufficiency. (2) In particular, the essential amino acids that are present in dietary protein are crucial for all biological processes including muscle synthesis, immune system function, and the production of hormones and neurotransmitters. Older adults tend to be at a higher risk for protein deficiency because they usually don’t consume enough dietary protein and the digestive system functions less efficiently with age.
Making sure you eat plenty of protein is helpful for combatting skin damage and wounds that result from venous insufficiency. Low-fat and nonfat meat, dairy, and egg whites are excellent sources of protein that contain optimal ratios of essential amino acids. However, limiting meat and dairy products may be helpful for reducing inflammation in individuals with chronic venous insufficiency. You can also get essential amino acids by eating a variety of plant proteins such as nuts, seeds, beans, and whole grains. Great examples of plant-based protein sources include lentils, chickpeas, almonds, walnuts, quinoa, tofu, flaxseeds, and whole-grain bread.
High-quality essential amino acid supplements may also be helpful by eliminating the hassle of making sure you eat a variety of protein sources, while also helping to increase absorption of essential amino acid in the digestive system. Before starting supplements, it’s a good idea to have them cleared by your physician.
3. Whole Grains
Whole grains are rich in fiber, minerals, and antioxidants that improve cardiovascular health and lower blood pressure. Whole grains are also an important source of plant protein. Why are whole grains better than refined grains? Whole grains contain the entire plant product, including the outer shell. The outer shell of whole grains is packed with fiber, antioxidants, and protein. When the starch component of the green is paired with these health-promoting components, the body breaks down the starch slowly, which provides a stable source of energy without spiking blood sugar levels.
In addition, the fiber and whole grains support a healthy and balanced gut microbiome, and good bacteria in the digestive system subsequently produce anti-inflammatory components that help fight inflammation in the cardiovascular system.
Excellent sources of whole grains to combat venous insufficiency include brown rice, quinoa, oats, buckwheat, whole-grain bread, and whole-grain pasta.
4. Healthy Fats
Certain dietary fats are very healthy and help reduce systemic inflammation, therefore improving vein function. Polyunsaturated fat and monounsaturated fats are the primary fats with anti-inflammatory properties. Omega-3 fatty acids are a type of polyunsaturated fat with potent anti-inflammatory compounds. Eating a diet rich in omega-3 fatty acids is connected to better heart health as well as the medication of numerous metabolic conditions such as insulin resistance, fatty liver disease, and type 2 diabetes.
Both plant and animal sources can provide healthy omega-3 fatty acids. Plant-based omega-3 fatty acids are available as alpha-linolenic acid, which is present in foods like walnuts, pecans, flaxseeds, and chia seeds. Oily fish is the best animal source of omega-3 fatty acids in the form of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). To incorporate more oily fish into your diet, eat foods like salmon, mackerel, sardines, arctic char, and anchovies.
5. Water
Drinking plenty of water is a great way to combat salt intake while keeping circulation up. Interestingly and somewhat counterintuitively, drinking lots of water helps combat fluid retention. Staying hydrated is key to making sure that all cellular processes progress smoothly. Keeping your fluid intake up is also important for flushing out waste products.
Diet for Venous Insufficiency: Food to Avoid
When following the diet for venous insufficiency, steer clear of inflammatory foods that worsen vein function.
1. Salty Foods
Eating too much sodium is a major contributing factor to conditions like high blood pressure and venous disease. Consuming lots of sodium causes water retention and drives up blood pressure. Eating too much salt on a daily basis can also worsen the swelling associated with venous insufficiency.
How can you reduce the amount of sodium you consume on a daily basis? High levels of salt are hiding in a number of foods that are commonly consumed in the traditional American diet. Food such as cheese, processed meat, frozen meals, canned food, and fried foods tend to be very high in sodium. Avoiding these meals and saving salt-laden foods as an occasional treat is an effective way to help manage chronic venous insufficiency.
Cutting salt out of your diet can help lower your blood pressure, improve vasodilation function, and overall improve circulation.
2. Saturated Fat
Saturated fat is a highly inflammatory compound for the circulatory system. Eating too much-saturated fat on a regular basis increases cholesterol levels, and is generally inflammatory for the circulatory system. High levels of cholesterol increase the risk of developing atherosclerosis, which in turn increases the risk of developing heart disease. Eating too much saturated fat is also linked to metabolic dysfunction and associated conditions such as fatty liver disease and type 2 diabetes.
Because of the inflammation that saturated fat can cause, cutting saturated fat out of your diet is an excellent way to improve circulation and fight against venous insufficiency. So what foods contain high levels of saturated fat? The main sources of saturated fat in the American diet include fatty dairy and meat products. To reduce the amount of saturated fat that you consume, steer clear of foods such as cheese, whole milk, cream, steak, and bacon.
3. Added Sugars
Added sugars are another inflammatory food that may worsen swelling in the lower legs and exacerbate venous insufficiency. What exactly does added sugar do to the body? Eating too much added sugar causes a flood of glucose to enter the bloodstream, which in turn spikes lead sugar levels.
Eating added sugars on a regular basis can over time cause metabolic dysfunction, including insulin resistance, fatty liver disease, and type two diabetes. Moreover, having chronically high levels or fluctuating levels of blood sugar can lead to significant inflammation in the arteries and veins. The inflammatory response throughout the circulatory system means that the endothelium doesn’t function as efficiently, worsening vein health and blood circulation.
Added sugars can be found in numerous food products, even if they don’t seem like they’re high in sugar. To reduce the amount of added sugar in your diet, steer clear of foods like candy, soda, cookies, ice cream, breakfast cereals, most granola bars, and pastries. Added sugars also tend to be hiding in foods like ketchup, salad dressing, and other sauces.
It’s also important to note that refined grains impact the body in the same way that added sugars do. Stay away from foods like white bread, white rice, and white pasta.
4. Dairy and Meat
High consumption of dairy and meat may increase systemic inflammation that worsens venous insufficiency. Eating too much dairy meat on a regular basis is associated with an increase of trimethylamine-N-oxide, which is a contributing factor for systemic information. In order to protect vein health, it’s a good idea to limit the amount of dairy and meat that you eat. When you do consume meat and dairy, stick to low-fat organic sources.
Lifestyle Changes for Venous Insufficiency
Although diet is extremely important for managing venous insufficiency, it is not the only tactic. Lifestyle changes can also make a significant difference by encouraging blood flow and
Regular Exercise
If you have chronic venous insufficiency, exercise is an important part of healing and encouraging blood flow. Exercise is important because it strengthens both your heart and the smooth muscle that lines your blood vessels and controls blood pressure. Incorporating regular exercise into your daily routine is helpful for both improving cardiac health and improving blood circulation.
If you are new to exercise and experience pain in your legs, it’s important to start out with gentle movements. Consult your doctor or physical therapist about exercises that help improve circulation without causing injury.
Elevation
Always having your lower legs positioned below your heart means that your veins must fight gravity to circulate blood. When the circulatory system is affected by venous disease, this isn’t so easy. Elevating your legs can improve circulation by using the force of gravity to allow blood and fluids to flow back towards the heart. Whenever you are sitting or lying down, keep your feet and legs comfortably elevated by propping them up on pillows and blankets.
Compression Garments
Compression garments are very helpful tools for fighting swelling and blood that pools as a result of venous insufficiency. Compression garments come in the form of bandages or stockings that squeeze the lower legs and help force fluids back towards the heart. Regularly wearing compression garments can help increase circulation and fight the symptoms of chronic venous insufficiency.
Skin Care
Skin wounds and ulcers are common symptoms of chronic venous insufficiency. Caring for these wounds increases your comfort and quality of life while helping the skin heal. Absorbent bandages and cream may help protect the skin and absorb any leakage. It’s also important to protect your skin from abrasions and other accidental injuries since the wound will take a long time to heal.
Other Treatment Options for Venous Insufficiency
In addition to diet and lifestyle changes, you may benefit from specialized procedures and surgery to help manage your symptoms.
Visiting a Vein Clinic
A vein clinic specializes in caring for individuals who suffer from vascular conditions. When you visit a vein clinic, you will undergo examinations and testing that evaluates vein function. Visiting a vein clinic is a great way to get specialized treatment for your condition.
Vascular Surgery
In many cases, venous insufficiency responds well to nonsurgical treatments like diet, lifestyle changes, and compression garments. However, in severe cases, undergoing vascular surgery may be the best way to treat venous insufficiency.
Vascular surgery is performed by vascular surgeons, who are specialized in treating conditions that affect the veins and arteries. A number of different surgeries may be performed to treat chronic venous insufficiency. The surgeon may use surgical techniques to repair damaged valves and remove damaged tissues. Or the surgeon may perform a valve replacement, in which damaged valves are removed and replaced with healthy valves.
Sclerotherapy
Sclerotherapy is a vein treatment that can be effective in treating varicose veins that arise as a result of chronic venous insufficiency. During a sclerotherapy procedure, a physician will inject a substance directly into the varicose veins. In the following weeks, the substance causes internal scarring within the veins, and blood is no longer able to travel through these veins, making them less visible. Blood flow will then travel through healthy veins.
Conclusion
Many of the strategies for improving venous insufficiency are also important for protecting your overall health. When striving to improve circulation and valve function, it’s very helpful to eat lots of fruits and veggies, high-quality protein, whole grains, and healthy fats. In addition to eating healthy foods, increasing physical activity, wearing compression garments, and elevating your legs are effective strategies for mitigating the symptoms of venous insufficiency. Vascular surgery is only recommended in severe cases of chronic venous insufficiency.
References:























