There are numerous types of chronic liver diseases. Chronic liver disease is a condition that pursues on a continuous basis and potentially leads to complications or more severe liver conditions. In this article, we explore different types of chronic liver diseases, common causes for chronic liver disease, the symptoms of chronic liver disease, and tips for managing liver disease. Read on to find out the answers to questions you might have about what it means to have chronic liver disease.
What Does It Mean to Have Chronic Liver Disease?
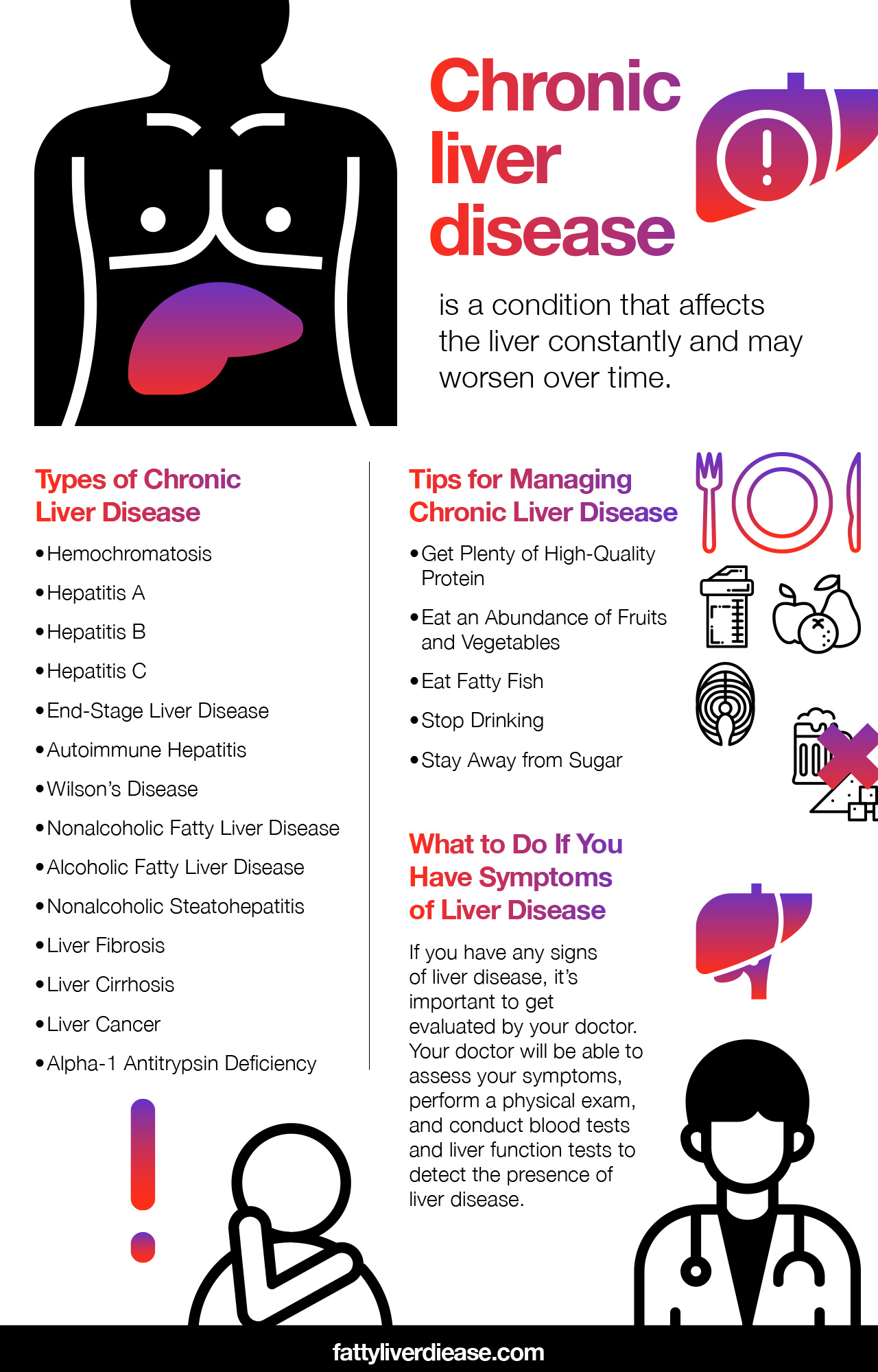
Chronic liver disease is a condition that affects the liver on a constant basis and may worsen over time. Chronic liver disease does not resolve spontaneously. There are numerous types of chronic liver disease that you may experience:
Hemochromatosis
Hemochromatosis describes a genetic liver condition in which your blood iron levels get too high, and iron deposits build up in the liver and other organs throughout the body. If you have hemochromatosis, your body is unable to process iron properly. Over time, high iron levels in the liver can cause damage and lead to more severe liver conditions like cirrhosis.
Hepatitis A
Hepatitis A is a viral infection that impacts the liver. Hepatitis A is rare in the United States because vaccines for the virus prevent widespread infection. However, hepatitis A may be more common in certain populations. Viral hepatitis A spreads through contact with contaminated food. Symptoms include malaise, nausea, lack of appetite, jaundice, and fever. In most cases, hepatitis A resolves within a few months, though it may also be a chronic condition with serious complications for at-risk individuals.
Hepatitis B
Like hepatitis A, hepatitis B is not common in the United States, and vaccination helps prevent the majority of cases. Hepatitis B often resolves on its own, though some infections may be chronic. Chronic hepatitis B can raise the risk of developing cirrhosis and hepatocellular carcinoma. Individuals may experience symptoms like jaundice, nausea, and fatigue.
Hepatitis C
Hepatitis C is a viral infection that transmits through blood or sexual fluids. Unlike hepatitis A and B, hepatitis C is not preventable by vaccination at this time. Hepatitis C causes inflammation in the liver, though it may be asymptomatic for many years. When left untreated, it can cause liver damage.
End Stage Liver Disease
End-stage liver disease signifies the most severe and progressed form of liver disease. If you have been diagnosed with end-stage liver disease, your liver is only retaining a tiny percentage of its function. If you have end-stage liver disease, a liver transplant is the most effective form of treatment. Liver transplantation involves replacing a diseased liver with a donated
Autoimmune Hepatitis
Autoimmune hepatitis is a non-viral form of liver inflammation. Autoimmune conditions are caused by immune system dysfunction. Usually, the immune system is designed to be a protective system that fights off bacteria and viruses while also halting malignant tissue growth. However, in the case of autoimmune hepatitis, the immune system malfunctions and cannot correctly distinguish invading or malignant particles from healthy tissue. As a result, the immune system begins to attack healthy tissue.
Wilson’s Disease
Wilson’s disease, like hemochromatosis, is a genetic condition that one is born with. Individuals with Wilson’s disease are unable to properly process copper. As a result, copper accumulates in the body and affects the liver. Wilson’s disease may initially be asymptomatic. However, as copper accumulates, the liver becomes inflamed. Over time, individuals with Wilson’s disease often develop a cirrhotic liver and may exhibit symptoms like jaundice, weight loss, and fatigue. Individuals with Wilson’s disease may also show signs of mental symptoms associated with copper accumulation in the brain as well as hepatic encephalopathy associated with liver damage.
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease, which is also referred to as NAFLD, describes the accumulation of fat in the liver due to diet and lifestyle factors, not alcohol consumption. Nonalcoholic fatty liver disease may also have a genetic component.
The foods that you consume influence your liver health significantly. Consuming foods that are high in refined grains, added sugar, and saturated fats are risk factors for developing nonalcoholic fatty liver disease. Obesity is also associated with nonalcoholic fatty liver disease. Metabolic conditions like type 2 diabetes and insulin resistance are also risk factors for developing nonalcoholic fatty liver disease.
Alcoholic Fatty Liver Disease
Alcoholic fatty liver disease describes the accumulation of fat in liver tissue due to alcohol consumption. Alcohol is a toxin that must be converted by the liver into its non-toxic form. Heavy alcohol use increases oxidative stress in the liver, which is the buildup of reactive free radicals in cells. These free radicals interact with healthy tissue and inflict damage. Chronic levels of oxidative stress contribute to inflammation and fat accumulation in the liver. Alcohol abuse increases the risk of developing fatty liver disease and other related liver conditions like alcoholic hepatitis.
Nonalcoholic Steatohepatitis
Nonalcoholic steatohepatitis (NASH) is a condition that indicates inflammation in the liver tissue. NASH is a progression of nonalcoholic fatty liver disease and is characterized primarily by inflammation. The best way to describe inflammation is by thinking about what happens when you injure yourself. For example, if you hit your knee, you will notice swelling, redness, and irritation in the affected area. Your immune system is activated and tending to the damage.
The same premise applies to inflammation in the liver. Essentially, an inflamed liver is swollen, irritated, and damaged. Symptoms of nonalcoholic steatohepatitis may include pain in the upper right quadrant, fatigue, and bruising.
Liver Fibrosis
Liver fibrosis is a condition characterized by the accumulation of tough collagen-based tissues in the liver. Fibrosis usually signifies the progression of either nonalcoholic or alcoholic fatty liver disease. As the liver endures chronic inflammation, tissues become damaged and eventually begin to scar.
Liver Cirrhosis
Continued liver fibrosis leads to the buildup of scar tissue in the liver and is the next stage in the progression of fatty liver disease. Causes of cirrhosis include alcohol abuse, poor diet, or genetic conditions. The scarring that is characteristic of cirrhosis creates areas of hardened, damaged tissue. These damaged areas are unable to carry out the normal functions of healthy liver tissue. Therefore, the damaged area of the liver is unable to effectively carry out its functions, which include the detoxification and metabolism of chemicals, synthesis of proteins, and production of digestive fluids.
Symptoms of cirrhosis include abdominal pain, lack of appetite, jaundice, and ascites.
Liver Cancer
Liver cancer, or hepatocellular carcinoma, is the growth of malignant cells within the liver. Cancerous cells are harmful and multiply uncontrollably until they take over an organ’s structure and function, causing end-stage liver failure. Liver cancer may also metastasize to other organs.
How does liver cancer develop, anyway? Liver cancer first develops with the growth of abnormal liver cells. When the DNA in liver cells is broken or damaged, cancerous or malignant cells can grow. DNA damage and abnormal cells are more likely to grow if liver tissue has been damaged by inflammation and oxidative stress. As a result, liver fibrosis and cirrhosis increase the risk of developing liver cancer.
Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin deficiency can lead to liver damage and dysfunction. Alpha-1 antitrypsin is a protein in the body that plays a role in preventing an inflammatory reaction in the lungs due to exposure to toxic chemicals like smoke and aerosols. Individuals with alpha-1 antitrypsin deficiency do not produce normal alpha-1 antitrypsin proteins. As a result, these abnormal proteins accumulate in the liver and increase the risk of developing liver disease. Dysfunctional alpha-1 antitrypsin proteins also increase the risk of developing lung conditions like chronic obstructive pulmonary disease (COPD).
Chronic Liver Disease Affects Liver Function
Any chronic liver disease is likely to cause hepatic impairment over time. In many cases, liver impairment is due to chronic inflammation and oxidative stress, which leads to scarring.
When only a small portion of the liver is damaged, the remaining healthy liver tissue can compensate for the scarred portion. However, as more liver tissue becomes damaged, the liver becomes overwhelmed. Early intervention in chronic liver disease is key to promoting liver repair and preservation of healthy liver tissue.
Many chronic liver diseases may not exhibit symptoms during the early stages of the condition. However, as damage progresses, liver function is compromised and causes symptoms. The symptoms of chronic liver disease tend to be similar, regardless of the origin of the condition. Liver disease symptoms include fatigue, nausea, loss of appetite, jaundice or yellow-tinted skin, unexplained weight loss, bruising, itching, ascites, spider angiomas or visible blood vessels, and mental symptoms like confusion during late stages.
Tips for Managing Chronic Liver Disease
If you have chronic liver disease, there are steps you can take to help support your liver at home. And, as always, it’s important to follow all medical advice that your doctor provides. There are also dietary and lifestyle changes you can make at home to support liver health. Many of the steps that you can take to prevent the progression of liver disease also help manage other conditions like metabolic syndrome. Here are a few steps you can take at home to support liver function.
Get Plenty of High-Quality Protein
Protein is a critical nutrient when you are healing from an injury or illness. When you have liver disease specifically, the body becomes more prone to muscle wasting. Getting plenty of protein helps fight against the side effects of fatty liver disease, liver fibrosis, and liver cirrhosis.
Essential amino acids seem to play a particularly important role in liver disease. The branched-chain essential amino acids play a critical role in regulating fat and sugar metabolism in the body. Research shows that branched-chain amino acids may protect against the worsening of liver diseases to hepatocellular carcinoma. (1) Moreover, these amino acids may help muscles utilize sugar and may be protective against insulin resistance. (1) In later stages of liver cancer, branched-chain amino acids may also prevent the worsening of cancer. (1)
Incorporating a high-quality essential amino acid supplement into your daily routine may help you get the amino acids you need to promote muscle growth. A high-quality essential amino acid supplement also provides essential amino acids in optimal ratios for the body to use.
Eat an Abundance of Fruits and Vegetables
Eating lots of fruits and veggies is one of the healthiest things you can do to support your liver. The antioxidants present in fruits and veggies have a protective effect on the liver, as well as other organs in the body. Antioxidants like polyphenols, carotenoids, and vitamin C help to neutralize free radicals in the liver. As a result, the liver can more readily repair itself and heal. Reach for fresh produce like spinach, beets, sweet potatoes, broccoli, blueberries, and blackberries.
Eat Fatty Fish
Fatty fish is high in omega-3 fatty acids, which are polyunsaturated fats with potent anti-inflammatory effects. The particular types of omega-3 fatty acids found in fish are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). In particular, salmon, mackerel, sardines, and Arctic char are rich in omega-3 fatty acids. Supplementing with a high-quality fish oil supplement is also a helpful way to get concentrated forms of omega-3 fatty acids. Always make sure your doctor approves your supplements.
Stop Drinking
Whether you have alcoholic fatty liver disease or not, alcohol is harmful to the liver. Especially when consumed in excess, alcohol causes oxidative stress and inflammation in the liver. Drinking alcohol will only worsen other liver conditions that you may have.
Stay Away from Sugar
Added sugar has been removed from its original source, heavily processed, and then added to other food products. Pastries, ice cream, soda, candy, and juice are packed with sugar. Plus, added sugar is hiding in many foods that we think of as staples in the American diet. For example, added sugar is a primary ingredient in many granola bars, breakfast cereals, condiments, yogurt, and bread.
Why is sugar so bad for the liver? When we eat added sugar, blood sugar levels skyrocket, and the body is unable to utilize all of the sugar at one time. Excess sugar is then deposited throughout the body in the form of fat. Over time, excess sugar consumption can lead to increased fatty deposits in liver tissue. Keep in mind that high blood sugar levels over time also cause inflammation throughout the body that can negatively influence your health in other ways.
What to Do If You Have Symptoms of Liver Disease
If you have any signs of liver disease or you have a genetic predisposition for liver disease, it’s important to get evaluated by your doctor. Your doctor can perform a variety of tests to confirm whether you have a liver condition. For example, a doctor will be able to assess your symptoms, perform a physical exam, and conduct blood tests and liver function tests to detect the presence of liver disease.
If needed, your internist will refer you to a hepatologist, a doctor who specializes in liver diseases. You may also visit a radiologist, who will conduct and interpret imaging of your liver.
If you have no symptoms, feel relatively healthy, drink only moderately or less, and eat a balanced diet, there’s no reason to suspect you have liver disease. This is especially the case if you get a routine check-up with bloodwork, which usually includes an evaluation of your liver enzymes.
What Do Liver Tests Look Like?
So, exactly what kinds of diagnostic tools are used when assessing the health of your liver?
First, a blood test will evaluate the levels of liver enzymes in your bloodstream. Specifically, blood tests may look at your levels of the liver enzymes aspartate transaminase (AST), gamma-glutamyl transpeptidase (GGT), and alanine transaminase (ALT). Elevated levels of liver enzymes signify inflamed liver tissue.
A physician may also use palpation or a physical examination to feel your abdomen and detect if your liver is enlarged. Enlargement of the liver signifies inflamed tissue.
Imaging tests provide a very accurate portrayal of what your liver tissue looks like. Ultrasound technology, magnetic resonance imaging (MRI), or computed tomography (CT) scans can all allow physicians to detect abnormalities in your liver tissue such as liver lesions or scarring. For example, an ultrasound can show the presence of fat accumulation within liver tissue.
A liver biopsy involves removing a very small sample of your liver to undergo testing and examination. A liver biopsy may reveal liver damage, liver cancer, fat accumulation, or liver lesions.
Follow Your Physician’s Advice
For conditions like Wilson’s disease, hepatitis, liver cancer, and liver failure, there are medications and treatments that are helpful for managing the conditions. Your doctor may recommend that you take medications like diuretics to help manage symptoms of liver disease, like cholesterol. Your physician may also advise that you avoid certain over-the-counter medications and supplements, such as acetaminophen or St. John’s Wort.
Conclusion
There are so many different kinds of chronic liver disease that can affect your liver’s function as well as your overall health. If you notice any signs of liver disease, it’s important to make an appointment with your doctor as soon as possible. Treating liver disease is easiest when caught during earlier stages. The liver is a very adaptable organ and responds readily to medical treatment, diet, and lifestyle changes that promote liver health.
References: