Maybe you are experiencing a dull aching pain under your right rib, which happens to be the area where your liver is located. Can your liver hurt? And what does liver pain mean? Here we answer all of the questions you may have about liver pain and associated conditions. Read on to find out more.
Liver Pain: What Does It Feel Like?
Liver pain may be perceived differently, depending on the individual. For some, liver pain may be felt in the upper right quadrant as a dull, persistent ache. For others, liver pain may feel like a stabbing or throbbing pain. Pain may also migrate to the right shoulder and the surrounding area.
Signs and Symptoms of Liver Disease to Look Out For
If pain in the right side under the ribcage is accompanied by other signs and symptoms of liver disease, it’s a good idea to seek medical attention to get to the root of the problem.
If you have liver pain, keep an eye out for these other signs and symptoms:
- Jaundice: Jaundice is a term that describes the yellowing of the skin. When the liver is inflamed and not working as it should, a compound called bilirubin builds up in the blood. This accumulation of bilirubin can cause your skin and the whites of your eyes to develop a yellowish hue.
- Loss of appetite: If you are suffering from liver damage or liver problems, it’s common to lose your appetite. Nausea is also common.
- Unintended weight loss: Liver damage alters metabolic processes, which can lead to unintentional weight loss.
- Muscle wasting: In cases of advanced liver disease like liver cirrhosis, loss of lean body mass is a common symptom.
- Fatigue: Feeling more tired than usual or weak is a sign that your liver may not be working as it should.
- Ascites and edema: Ascites describes the accumulation of fluid in the abdomen, while edema describes fluid retention. For individuals with liver damage, edema most commonly occurs in the legs. Liver damage can impede the passage of blood through the portal vein that’s present in the liver. As a result, fluid collects in the abdominal area and lower extremities.
- Itchy skin: Itching in association with liver disease is most common when the biliary duct system is affected. Biliary ducts are responsible for facilitating bile flow from the liver to the gallbladder and small intestines. When these ducts are damaged or inflamed, bile salts may collect beneath the skin and result in chronic itching.
- Hepatic encephalopathy: hepatic encephalopathy occurs in advanced cases of liver disease. When the liver is so damaged that it can’t detoxify and process compounds, these toxic compounds enter the bloodstream and travel throughout the body. Ammonia in the brain can cause severe mental symptoms like confusion, anxiety, slurred speech, and seizures.
Risk Factors for Developing Liver Disease
In many cases of early liver disease, you may not experience any symptoms at all. Maybe a dull right upper quadrant pain is the only symptom you experience. However, several risk factors increase your probability of developing liver disease.
- Insulin resistance and type 2 diabetes: Insulin resistance and type 2 diabetes signify that your metabolism isn’t working properly. As a result, the body is unable to keep blood sugar levels at a healthy level. Sugar present in the blood is readily turned into fat and deposited throughout the body, including the liver.
- Obesity: Being overweight is a risk factor for systemic inflammation, heart disease, and fatty liver disease. Excess fat deposits throughout the body also increase the risk of having a fat buildup in liver tissue.
- Alcohol abuse: If you regularly or chronically drink excess alcohol, you are at a higher risk of sustaining liver inflammation and damage. Excess alcohol consumption is defined as having more than two drinks per day for men and more than one drink per day for women. The liver is responsible for processing and detoxifying all of the alcohol we consume. Excess alcohol can overwhelm the liver and increase oxidative stress and inflammation.
- Family history of liver disease: Your genetics influence the likelihood of developing liver conditions. If liver conditions run in your family, you may be at a higher risk of developing liver disease.
When You Shouldn’t Worry
If you are generally in good health, are younger, don’t drink excess alcohol, and don’t have a metabolic condition, the risk of having liver disease is low. However, if you are worried, it’s always a good idea to get checked out.
What Diagnosis of Liver Disease Looks Like
In any case, if you are experiencing persistent abdominal pain that you’re worried about, it’s a good idea to go to the doctor to get it checked out. Undergoing tests and evaluation by a doctor can help you get peace of mind or address any problems if necessary.
A physician may be able to detect liver abnormalities using a tactic called palpation. Your doctor may be able to feel the enlargement of the liver or the presence of abnormal growths and nodules.
Your doctor will also order blood tests, which can detect the levels of liver enzymes in the bloodstream. Elevated levels of liver enzymes signify inflammation.
Imaging tests are also very valuable diagnostic tools for managing fatty liver disease. Ultrasounds, computed tomography (CT scans), and magnetic resonance imaging (MRI) tests can reveal abnormalities in liver tissue like fat particles, nodules, and an enlarged liver. A type of ultrasound technology called elastography can even reveal information about the texture of liver tissue.
Finally, a liver biopsy is one of the most accurate ways to detect and diagnose liver disease. A liver biopsy involves removing a tiny sample of tissue from your liver and having it examined for the presence of fat, scar tissue, and other abnormalities.
Potential Causes of Liver Pain
There are many liver conditions that can cause pain, inflammation, and damage in the liver. Here we go through the possible causes of liver pain.
Non-Alcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease describes the accumulation of excess fat within liver cells. It develops as a result of metabolic dysfunction and a diet high in saturated fat and sugar. Though initially not accompanied by any symptoms, non-alcoholic fatty liver disease may progress to more serious forms of liver disease, causing symptoms like liver pain, ascites, jaundice, and weight loss.
Alcoholic Fatty Liver Disease
Can your liver hurt after drinking alcohol? Alcohol use may exacerbate inflammation in the liver. In particular, alcoholic fatty liver disease also causes a buildup of fat within liver cells, although the pathogenesis results from chronic alcohol consumption and not from metabolic dysfunction. Continued alcohol consumption accelerates alcoholic fatty liver disease progression to more severe liver conditions, like steatohepatitis, fibrosis, and cirrhosis.
So, can your liver hurt from drinking alcohol? Yes, your liver can hurt from drinking alcohol, especially if you have alcohol-related liver disease.
Steatohepatitis
Steatohepatitis describes a state of inflammation that occurs after you’ve had fatty liver disease for a prolonged period of time. Once fatty liver disease has progressed to steatohepatitis, you may notice more symptoms. It also becomes more likely that your case of fatty liver disease will progress to fibrosis and cirrhosis.
Fibrosis and Cirrhosis
Fibrosis describes the accumulation of tough, fibrous tissue around liver cells due to chronic inflammation and damage. Over time, fibrosis may lead to liver cirrhosis. Liver cirrhosis is a severe form of liver disease characterized by scarring of liver tissue. A cirrhotic liver is very hard in texture since hardened scar tissue healthy liver tissue. Scarred areas of the liver are no longer able to carry out normal functions. Significant scarring of the liver seriously compromises liver function.
Liver Abscess
A liver abscess is a collection of pus and bacteria in the liver. A liver abscess may develop as a secondary symptom to another condition such as diverticulitis or acute liver injury. Treating a liver abscess requires medical intervention, and you will most likely need to take antibiotics and undergo a drainage process to rid your liver of pus.
Viral Hepatitis
Viral hepatitis may be a cause of liver pain. Hepatitis A and hepatitis B may cause chronic liver disease. However, the most common form of viral hepatitis in the United States is hepatitis C. Hepatitis C is contracted through sexual contact or exposure to contaminated blood. Over time, chronic infection with hepatitis C may cause inflammation and subsequent damage.
Liver Failure
Liver failure is the most advanced form of liver disease, when the liver has lost nearly all of its ability to function. Liver cancer and advanced liver cirrhosis are common causes of liver failure. At this point, liver disease is immediately life-threatening, past the point of treatment, and requires a liver transplant. Liver failure is accompanied by very severe symptoms, including extreme weakness, jaundice, ascites, and hepatic encephalopathy.
Gallbladder Issues
Gallbladder problems may cause liver pain. When gallstones form in the gallbladder, they can block bile flow through bile ducts. Gallstones can cause an accumulation of fluid and bacteria in the liver, causing inflammation and pain. Gallstone attacks that are causing disruptive symptoms often require treatment by removing the gallstones or a cholecystectomy, which is the complete removal of the gallbladder.
Autoimmune Hepatitis
Liver problems and liver pain may be a result of autoimmune hepatitis. Autoimmune hepatitis is a condition in which the immune system doesn’t function as it normally should. This means that the immune system attacks healthy liver tissue, causing damage, inflammation, and subsequent pain.
Hemochromatosis
Hemochromatosis is a genetic condition that can eventually result in liver inflammation, cirrhosis, and liver pain. Individuals with hemochromatosis absorb an unusually high level of iron from the foods they eat. Excess iron is then deposited throughout the body, including the joints, heart, and liver. Over time, accumulated iron causes liver inflammation and subsequent pain.
Chemical Liver Damage
Certain medications are associated with liver damage. For example, taking too much acetaminophen or combining acetaminophen with alcohol can lead to serious liver damage. However, when acetaminophen or Tylenol is used as directed, they rarely cause any issues. Statins are another class of medications used to control the levels of cholesterol and triglycerides in the bloodstream. Rarely, statins may be associated with liver inflammation.
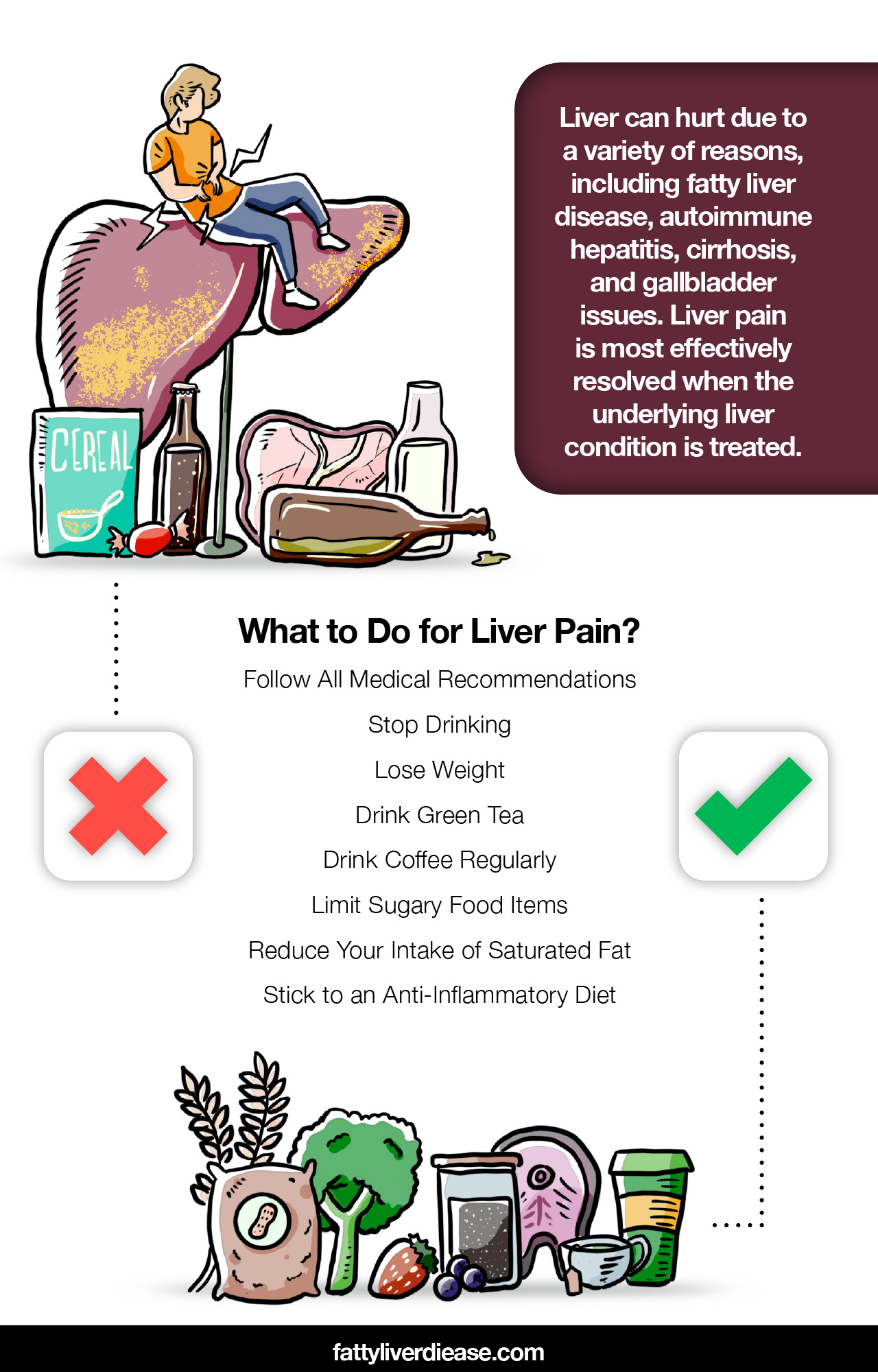
What to Do for Liver Pain
Liver pain is most effectively resolved when the underlying liver condition is treated. Here we go through what you can do to manage your liver condition, including diet, lifestyle changes, and other recommendations.
1. Follow All Medical Recommendations
It’s essential to follow all medical advice and treatment plans provided by your physician. Different cases of liver disease often require specific medical treatments and protocols. Following medical recommendations for treating your liver condition is vital for resolving any liver pain you are experiencing.
For example, viral hepatitis C requires taking regular doses of antiviral medication. Managing autoimmune hepatitis may require taking immunosuppressants regularly. It’s also imperative to clear all diet and lifestyle changes with your doctor, to make sure you’re taking the right steps to support liver health.
2. Stop Drinking
If you are a heavy drinker, it’s vital to cut alcohol out of your diet. If your liver pain results from alcoholic fatty liver disease, you may notice an improvement in your symptoms following cessation of drinking. While you are drinking, the body is unable to allocate energy and resources towards repairing damage and must instead focus on breaking down alcohol and eliminating it from the body. Quitting alcohol consumption allows your body to heal from alcohol-induced inflammation effectively.
If you are a chronic drinker, be careful to avoid quitting cold turkey. Physical reliance on alcohol requires a slow tapering of alcohol consumption, combined with medical supervision. If you plan to detox from alcohol, it’s a good idea to talk to your doctor about the best way to eliminate alcohol from your daily routine. Inpatient treatment may also be required. You can also discuss the option of at-home detoxing with regular outpatient monitoring.
3. Lose Weight
If you are overweight and have non-alcoholic fatty liver disease, losing weight is an effective way to improve liver health. Obesity is a major risk factor contributing to the development of fatty liver disease. The increase of fatty deposits throughout the body also increases fat deposits within the liver.
Research shows that weight loss is a beneficial strategy for individuals with non-alcoholic fatty liver disease. A systematic review and meta-analysis published in JAMA Internal Medicine evaluated 22 studies that examined the impact of weight loss on non-alcoholic fatty liver disease. (1) Results revealed that weight loss was connected to a decrease in liver enzyme levels and less fat accumulation in the liver. (1)
If you are aiming to lose weight for fatty liver disease, it’s a good idea to eat a balanced diet and increase your physical activity.
4. Drink Green Tea
Adding a cup of green tea to your daily routine can be an effective way to enhance the antioxidant content of your diet. Green tea is loaded with antioxidant compounds like polyphenols and catechins. Try drinking green tea either hot or chilled. You can also add green tea to smoothies and juice with little or no impact on flavor.
5. Drink Coffee Regularly
A regular cup of coffee or two may help decrease liver inflammation and protect the liver from further damage. It’s important to make sure that your coffee doesn’t contain lots of unhealthy additives like sugar and cream, which can actually worsen fatty liver disease. Instead, stick to black coffee and plant-based creamers that are low in both sugar and fat.
6. Limit Sugary Food Items
Added sugar is rampant in so many foods that we eat. For example, we can find added sugars in pastries, soda, candy, breakfast cereal, condiments, and other packaged food items. Eating foods high in sugar can significantly contribute to fatty liver disease. Eating a meal rich in sugar sends blood glucose levels soaring. Because body cells cannot effectively utilize the glucose, the sugar is deposited throughout the body as fat. The chronic consumption of foods high in added sugar also worsens metabolic function and contributes to fatty liver disease risk factors, like insulin resistance and type 2 diabetes.
7. Reduce Your Intake of Saturated Fat
Saturated fat is abundant in foods like pork, steak, bacon, salami, lunch meats, hard cheese, whole milk, and cream. Eating a diet rich in saturated fat can seriously interfere with healthy metabolic functioning and contribute to fatty liver disease. Saturated fat interferes with normal insulin function, which causes the body to process sugar inefficiently. To support the reversal of fatty liver disease and reduce liver pain, it’s important to decrease your saturated fat intake. When consuming meat and dairy products, always choose the products that are low-fat or nonfat.
8. Stick to an Anti-Inflammatory Diet
Eating an anti-inflammatory diet is an important component of managing liver disease, especially non-alcoholic fatty liver disease. An anti-inflammatory diet includes plenty of whole foods, while minimizing packaged and processed foods. The primary components of an anti-inflammatory diet include fruits and veggies, nuts, seeds, beans, whole grains, fatty fish, and smaller portions of lean meat and dairy.
Fruits and Veggies
Fruits and veggies are a critical part of a liver-friendly diet because they are rich in vitamins and antioxidants. The vitamins and antioxidants present in fresh produce directly combat oxidative stress in the liver. For example, polyphenols can neutralize free radicals that build up in liver tissue due to oxidative stress from liver disease. Reach for produce like broccoli, spinach, strawberries, and blueberries.
Nuts and Seeds
Nuts and seeds are excellent sources of vitamins, minerals, antioxidants, healthy fats, and protein. The healthy fats present in nuts and seeds are polyunsaturated, and they have a profoundly different effect on the body than saturated fats. Eating plenty of polyunsaturated fats is vital for supporting healthy metabolic function and a healthy liver. Pecans, walnuts, flaxseeds, and chia seeds are particularly rich in polyunsaturated fats called omega-3 fatty acids. The type of omega-3 fatty acids present in nuts and seeds is alpha-linolenic acid (ALA).
Whole Grains and Beans
Whole grains and beans are packed with fiber that is vital for supporting digestive health, and subsequently liver health. Eating a diet high in dietary fiber helps balance the microbiome in the gut. When healthy bacteria populate the gut, these bacteria release anti-inflammatory compounds that are absorbed through the digestive tract and into the bloodstream. These anti-inflammatory compounds can then travel to the liver and help repair damaged and inflamed tissue.
Protein
High-quality protein is a critical part of a liver-friendly diet. Protein offers amino acids, which are the building blocks of all proteins. In particular, high-protein food sources provide essential amino acids, which are nutritionally required for humans because the body cannot synthesize these amino acids internally. The human body requires optimal ratios of these essential amino acids on a daily basis. Certain essential amino acids also play an important role in helping support healthy metabolic functions and lower inflammation in the liver. (2)
Lean meats and dairy products provide optimal ratios of essential amino acids, as well as fatty fish. Vegetable proteins are incomplete proteins. To get optimal ratios of essential amino acids from plant-based sources, it’s important to eat a variety of vegetable protein throughout the day. In later stages of liver disease, essential amino acids can help combat muscle wasting and fatigue.
Oily Fish
Individuals with liver disease may also benefit from eating oily fish like salmon and mackerel. Fatty fish contain an abundance of omega-3 fatty acids in the form of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Omega-3 fatty acids from fish are potent anti-inflammatory agents and help decrease systemic inflammation as well as inflammation in several organ systems, like the liver.
Conclusion: Can Your Liver Hurt?
In a nutshell, your liver can hurt due to a variety of reasons, including fatty liver disease, autoimmune hepatitis, cirrhosis, and gallbladder issues. Inflammation and damage can cause liver pain in the upper right quadrant of your abdomen, under the ribs. To determine the cause of the pain, it’s always a good idea to see your doctor and get a diagnosis and treatment plan. Treating the cause of liver pain is the best way to manage liver pain. Diet and lifestyle changes are an integral part of treating liver conditions and associated pain.
References: