A couple of drinks every now and again is generally harmless and may even be associated with health benefits. But what happens when you overdo it? Drinking too much alcohol can wreak havoc on your organs, particularly the liver, and result in the development of the alcoholic fatty liver disease. Can the liver regenerate and recover from prolonged, heavy drinking?
How Does Alcoholic Liver Disease Compare to Nonalcoholic Liver Disease?
Let’s first distinguish the alcoholic fatty liver disease from nonalcoholic fatty liver disease. Both forms of fatty liver disease are defined by the accumulation of fat in the liver, also called hepatic steatosis.
Both diseases progress in a similar manner. If hepatic steatosis continues without adjustments to diet and lifestyle, fatty liver disease can progress to steatohepatitis, which is characterized by liver inflammation. If left unchecked, both alcoholic and nonalcoholic may progress to liver fibrosis, cirrhosis, hepatocellular carcinoma (liver cancer), and ultimately liver failure.
However, the likelihood of disease progression seems to be markedly different for those with alcoholic and nonalcoholic fatty liver. In a study published in the Scandinavian Journal of Gastroenterology, researchers conducted a 20-year follow-up with either alcoholic or nonalcoholic fatty liver disease. Results found that 1.2% of patients with nonalcoholic fatty liver disease and 22% of patients with alcoholic fatty liver disease progressed from simple hepatic steatosis to cirrhosis. Researchers also observed that mortality among patients with alcohol-induced fatty liver was directly connected to liver damage and alcohol, while mortality among patients with nonalcoholic fatty liver was more connected to comorbid conditions like heart disease and cancer. (1)
The causes of fat accumulation and the clinical presentation have significant differences.
Alcoholic fatty liver disease develops as a result of continuous, heavy drinking. Alcohol in high doses is a poison that is a stressor to all the cells throughout your body. The liver, however, takes a direct hit since it functions as your body’s processing plant. All alcohol that you ingest is passed through the liver, where enzymes like cytochrome p450, alcohol dehydrogenase, and aldehyde dehydrogenase detoxify ethanol into substances that can be safely excreted from the body.
However, the liver is unable to directly process alcohol into benign products. Instead, alcohol first becomes acetaldehyde, and then acetate. Acetaldehyde is a particularly harmful compound that damages liver cells. Free radical species are also significant byproducts of the alcohol metabolism pathway, contributing to inflammation and fat accumulation in the liver.
Can periodic binge drinking contribute to fatty liver disease? Binge drinking is certainly unhealthy, but the research mainly shows that the risk of alcoholic fatty liver disease is largely determined by chronic, heavy drinking that takes place on a daily basis.
On the other hand, nonalcoholic fatty liver disease develops as a direct result of the continuous consumption of excess calories, sugar, and saturated fat. Nonalcoholic fatty liver disease is described as a metabolic disorder that is usually grouped with other metabolic conditions like obesity, type 2 diabetes, and insulin resistance.
Risk Factors Associated with Developing Alcoholic Fatty Liver Disease and Nonalcoholic Fatty Liver Disease
Interestingly, even though the alcoholic fatty liver disease is caused by continuous heavy alcohol consumption, not all heavy drinkers will develop the condition. Similarly, not every individual with above-average BMI and metabolic conditions will develop nonalcoholic fatty liver disease.
Research shows that the risk factors for developing both alcoholic and nonalcoholic fatty liver disease are similar. For both forms of fatty liver disease, the same gene – PNPLA3 – raises the risk of developing the condition and progressing to more damaging forms of liver disease. Other overlapping risk factors include old age, obesity, and conditions associated with metabolic syndrome. (2)
Because of the overlap in risk factors for developing both forms of fatty liver disease, it can be suggested that many curative steps for one form will be effective for the other form as well.
Can the Liver Heal Itself?
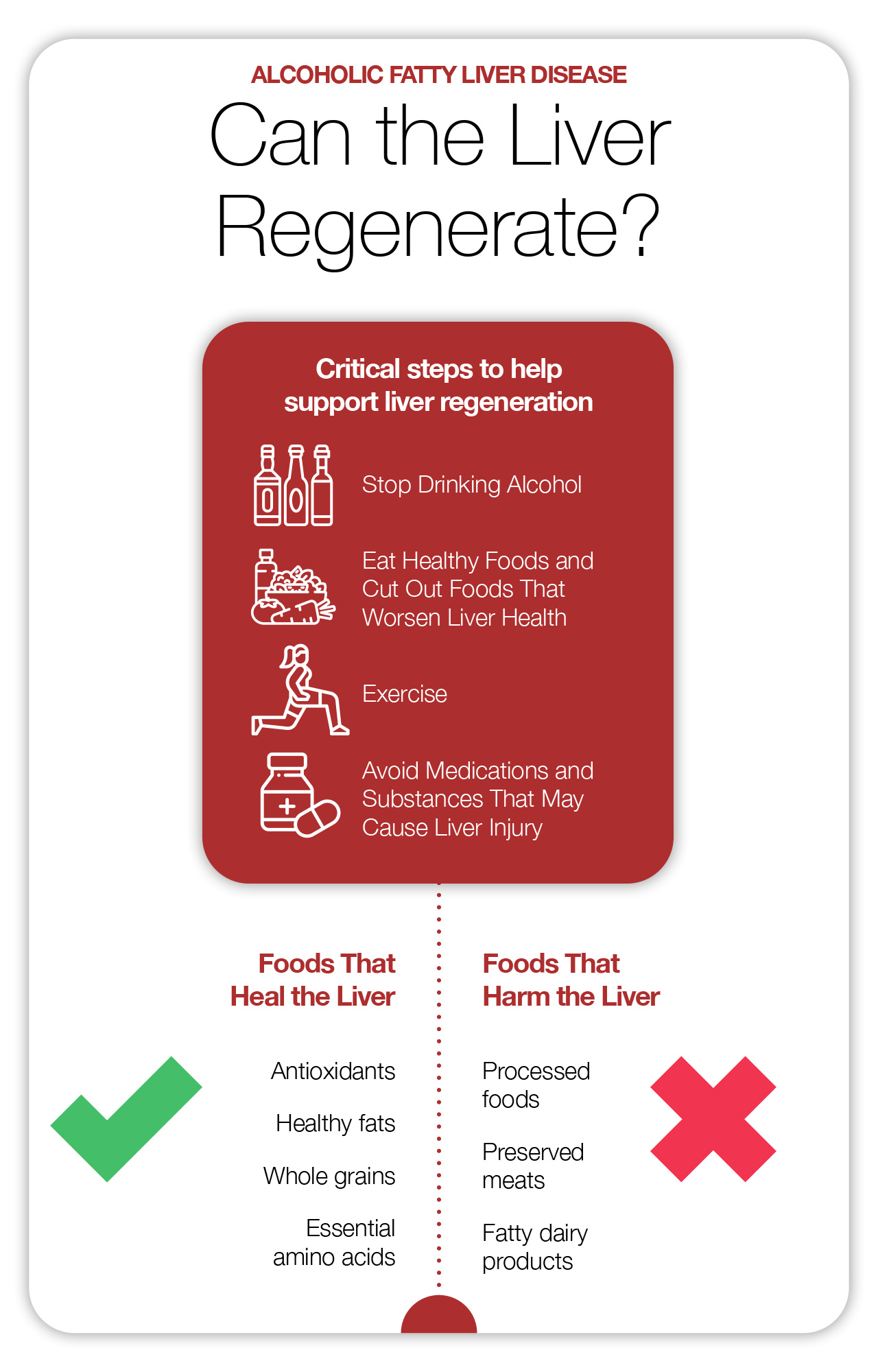
The liver is remarkably adaptable and is able to effectively regenerate, regrow, and repair. The level of regeneration is dependent on the extent of liver injury. When it comes to the early stages of alcoholic fatty liver disease, here are the critical steps to supporting the restoration of liver functions.
1. Stop Drinking Alcohol
This one is much easier said than done. Alcoholism is a disease that is characterized by the compulsive consumption of alcohol that interferes with normal functioning. Recovering from alcoholism is a long-term process that starts with detox. Detox is a critical first step that rids the body of alcohol and breaks the body’s physical dependency on alcohol. The next steps usually include a mix of inpatient treatment, sober living, and mental health counseling. Maintaining sobriety can be a challenging, life-long journey. Make sure you have the support of close friends, family members, and support groups that can keep you accountable and can provide stability and encouragement throughout the process.
To help the liver repair from alcohol-induced damage, it is crucial to remain sober. Diet and lifestyle changes that promote liver repair will be fruitless without first addressing the core cause of fatty liver disease in the first place. Continued heavy drinking significantly raises the risk of developing chronic liver disease and serious complications.
2. Eat Healthy Foods and Cut Out Foods That Worsen Liver Health
Since both alcoholic fatty liver disease and nonalcoholic fatty liver disease share some common risk factors, the same diet changes will be effective for reducing inflammation and promoting liver repair for both conditions.
Foods That Heal the Liver
- Antioxidants: In order to support liver repair, make antioxidants a focus in your diet. Antioxidants are micronutrients that are present in natural, whole foods like fruits, veggies, whole grains, nuts, and seeds. Vitamin C, polyphenols, and carotenoids are examples of the kinds of antioxidants that can be found in food. These compounds are your body’s healers and protectors that disarm free radicals and prevent oxidative damage. Antioxidants promote the smooth functioning of the immune system to ensure that liver cells get repaired efficiently. Other compounds found in turmeric and green tea support the liver in reversing alcohol-related damage and fight against disease progression. Potent antioxidants help prevent fibrosis and the accumulation of scar tissue in cirrhosis.
- Healthy fats: When it comes to fats, the best kinds are polyunsaturated and monounsaturated fats. These healthy fats can be found in plant foods as well as fatty fish. Healthy plant-based sources of fats include avocado, walnuts, almonds, flaxseeds, chia seeds, and pecans. Flaxseeds and chia seeds contain essential amino acids as well as the alpha-linolenic acid (ALA), a plant source of omega-3 fatty acids. Fatty fish are rich sources of docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). All forms of omega-3 fatty acids attenuate liver damage and protect against inflammation and further disease progression.
- Whole grains: Whole grains are filled with fiber, antioxidants, and complex carbohydrates that sustain energy and stabilize blood glucose levels. The fiber in whole grains is critical to promoting gut health by feeding healthy gut bacteria that produce anti-inflammatory byproducts. These anti-inflammatory compounds travel through the body and influence liver repair and brain health. Whole-grain fiber may play a role in repairing alcohol-related gut damage. Additionally, whole grains stabilize blood sugar, facilitate weight loss, and promote insulin sensitivity.
- Essential amino acids: Essential amino acids are the smallest components of protein that humans require through dietary sources. There are 10 essential amino acids that can be produced by the body, and 9 essential amino acids that must be absorbed from nutritional sources. The nine essential amino acids are critical to maintaining homeostasis throughout the body and strengthening the immune system, promoting healing and cellular repair, synthesizing neurotransmitters, and boosting muscle synthesis and metabolism. Certain essential amino acids, like the branched-chain amino acids, play a critical role in reversing malnutrition and muscle loss associated with advanced liver disease. Essential amino acids are present in many food sources, including nuts, seeds, whole grains, dairy products, and meats. However, the only sources that contain all essential amino acids in optimal ratios are dairy products, meats, and soybean products like tofu and tempeh. If you want to get all essential amino acids from vegetable sources only, it’s important to eat a variety of plant-based protein sources that complement one another.
Foods That Harm the Liver
- Processed foods: Processed foods are generally high in added sugars, saturated fat, sodium, and preservatives that will exacerbate liver inflammation and cause fat to build up in the liver. These foods could potentially turn a case of alcoholic fatty liver disease into nonalcoholic fatty liver disease. To support liver recovery, avoid packaged and processed foods like cookies, crackers, cakes, ice cream, candy, white bread, white rice, and other baked goods and processed items.
- Preserved meats: Many meats have been packed with preservatives like artificial nitrates and excess sodium. Nitrates interact with the protein in meat to produce inflammatory compounds that may inflict or worsen liver damage. Meats are also a major source of saturated fat, which negatively influences metabolic function. To promote optimal healing from alcohol-induced liver damage, steer clear of meats like bacon, sausage, deli meats, and canned meats.
- Fatty dairy products: Dairy can be a significant source of saturated fat. Stay away from full-fat dairy products like cream, butter, cheese, and milk, and instead opt for the nonfat versions. When buying packaged dairy products, be sure to check the ingredients list and nutrition label as well. Many yogurts contain lots of added sugar, while cheese can be very high in sodium. Only choose low-sugar and low-sodium dairy foods. Nonfat, low-sugar Greek yogurt is an excellent option to get all essential amino acids while forgoing harmful fats that are bad for liver health. Nonfat mozzarella cheese is an excellent high-protein cheese option that contains minimal amounts of sodium.
3. Exercise
Exercise is critical in supporting cardiovascular health and increases blood flow to all organs, including the liver. Improved blood flow ensures that the liver is supplied with plenty of oxygen, antioxidants, vitamins, and minerals that it needs to repair. Plus, exercise can facilitate weight loss and mitigate risk factors for fatty liver disease like insulin resistance and type 2 diabetes, which in turn can help reverse fatty liver disease.
A study conducted by Japanese researchers assessed the protective effects of alcohol among individuals who never drink, drink moderately, or drink heavily. Results found that for individuals who never drink and drink moderately, exercise exerted liver-protecting effects and lowered the risk of developing fatty liver disease. However, no such association was found for heavy drinkers. (3)
This research underscores the importance of first eliminating alcohol consumption, and then adding exercise to your regimen. Exercising while drinking heavily likely has no effect on reversing fatty liver disease.
4. Avoid Medications and Substances That May Cause Liver Injury
Some medications can exacerbate liver inflammation and cause liver injury. In particular, the popular over-the-counter painkiller acetaminophen has the potential to cause liver injury if taken in high doses. Acetaminophen is also particularly harmful to the liver when taken in combination with alcohol.
Other medications that could cause liver injury include certain antibiotics, antifungal medications, and antiviral medications for the management of HIV. Statins, which are often used in the management of high cholesterol levels, can also cause inflammation in the liver. If you’re experiencing liver problems in response to medications, your physician will likely be able to find an effective alternative medicine that treats your condition without compromising liver function.
Some herbs, like kava root, may also cause liver inflammation, liver injury, and lead to serious liver problems. (4)
How to Know If You Have Alcoholic Fatty Liver Disease
It can be difficult to tell whether your form of fatty liver disease is alcohol-related or nonalcoholic, and that determination is best left up to a doctor.
If you’re worried you may have fatty liver disease related to alcohol, you may notice some of the following symptoms:
- Liver pain after drinking
- Fatigue
- Loss of appetite
It is possible that you may not have any symptoms of early stages of alcoholic fatty liver disease, or that the symptoms you do have are masked by continuous alcohol consumption.
How Long to Abstain from Alcohol to Repair Liver Damage?
If you’re in the early stages of fatty liver disease, abstaining from alcohol will likely improve liver damage and inflammation in just a matter of weeks.
If your fatty liver disease has progressed to alcoholic steatohepatitis, fibrosis, or cirrhosis, it will take months or years for your liver to repair damage and regain liver function. In many cases, especially in the case of cirrhosis, it is unlikely that your liver will be able to make a full recovery. However, a healthy fraction of the liver that is supported by a healthy diet and alcohol-free lifestyle can support the entire body, even if the rest of the liver is damaged.
Later Stages of Alcoholic Liver Disease
If early stages of fatty liver disease have progressed to more advanced forms of liver disease, symptoms will be more severe since liver function is more compromised.
Symptoms of liver fibrosis and cirrhosis include jaundice, ascites, water retention, bruising, unintentional weight loss, enlarged blood vessels, itchy skin, confusion, and in severe cases, hepatic encephalopathy.
Liver Regeneration in Later Stages of Alcoholic Liver Disease
If alcoholic liver disease has progressed to liver cirrhosis, some liver regeneration is still possible, depending on the severity of liver damage. The human liver is a remarkable organ because it has the most regenerative capacity of any organ in the body. Even an adult liver that has passed the stage of growth and development is able to regenerate.
Hepatic regeneration is triggered in response to trauma or liver injury. For example, a cancerous liver mass may require the surgical removal of a section of the liver, a procedure called a partial hepatectomy. Or, scar tissue may be compromising liver function as a result of alcohol-induced liver cirrhosis.
study shows that in response to hepatic injury, biliary epithelial cells produce new hepatocytes. (5) These new hepatocytes, or liver cells, can enter the cell cycle in response to injury and undergo rapid cell division. Once cell division has been initiated, hepatocyte growth factors are activated to support the proliferation of new hepatocytes. The two growth factors that are responsible for facilitating liver regeneration are c-met and epidermal growth factor receptors. Proliferating liver cells ensure that millions of new, healthy liver cells are produced. Once sufficient numbers of healthy cells have been produced, the cell cycle ceases.
Stem cell research is a growing area within hepatic regenerative medicine. Stem cells have been studied as a possible option to support liver regeneration in cases of liver cirrhosis and end-stage liver failure, and has been used successfully as a form of treatment. Stem cells are essentially “blank slates” that can grow and develop to form tissues and organs with specialized functions, to replace damaged tissues.
Research has been exploring the possibility of generating new liver tissues through stem cells. At this time, conventional liver transplantation is still the safest and most effective treatment for liver tumors, end-stage liver failure, and late-stage cirrhosis. (6) However, stem cell therapy for liver regeneration holds promise for the future.
The curative steps discussed above that support healing from alcoholic fatty liver disease, also support hepatic regeneration in response to more severe liver diseases and liver damage like fibrosis, cirrhosis, liver cancer, and end-stage liver disease. Antioxidants and essential amino acids support healthy immune function and efficient tissue repair.
Conclusion
Does the liver regenerate? Absolutely. In the early stages of alcoholic fatty liver disease, quitting drinking and making healthy diet choices are likely sufficient to facilitate a full recovery. However, in late-stage alcoholic liver disease when liver function is severely compromised and unable to recover, liver transplantation is the best option. If you’re concerned you may be suffering from alcoholic fatty liver disease, talk to your health care provider about medical interventions. A healthy, liver-friendly diet that supports healing and repair will be important for liver regeneration in all cases of liver disease.
References:
(1) https://www.ncbi.nlm.nih.gov/pubmed/19670076/
(2) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4093692/
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127917/
(4) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3160634/























