When a person has liver dysfunction for a long time, it can cause Hepatic Encephalopathy (H.E). This happens because the person’s liver can no longer effectively clear out toxic products off the body. Experts are yet to establish the particular toxins that lead to H.E. But then, ammonia may have something to do with it. Many doctors even use ammonia levels as one of the indices to diagnose hepatic encephalopathy. They even use it to guide them in their treatment regimen. Ammonia level in hepatic encephalopathy is very important. Aside from its levels, doctors also use it partial pressure to determine how severe a person’s hepatic encephalopathy is.
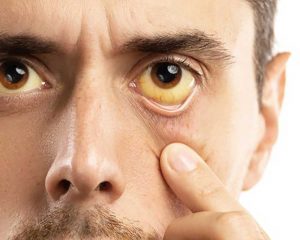
What Is Hepatic Encephalopathy?
Hepatic Encephalopathy is not just one dysfunction. It is a variety of neuro and psychiatric dysfunctions. But these dysfunctions can be reversed. This condition occurs in people who have liver dysfunction. But doctors can only say you have H.E when they rule out any other metabolic and/or neurologic dysfunction.
The word, “Hepatic” shows that the dysfunction originates from the liver. The term, “Encephalopathy”, on the other hand, shows that brain function has been altered. So together, the term implies some form of alteration in brain function as a result of liver dysfunction. When the liver can no longer remove certain toxins from your body, the toxins can enter into the brain and cause dysfunctions. But as soon as you can improve liver functions, the symptoms will reverse.
Ammonia Level in Hepatic Encephalopathy
Ammonia is a byproduct that comes from the breakdown of nitrogen. When your body breaks down any compound that contains nitrogen, it produces ammonia. But when ammonia levels are too high, it becomes toxic to your brain.
Now, your liver is the organ that helps to clear almost all the ammonia in your portal vein. It detoxifies as much as 85 percent of all the ammonia your body produces. It converts the ammonia into urea and glutamine. This prevents the ammonia from entering into your systemic circulation.
When there is impairment in your liver function, what happens? The liver will not be able to remove enough ammonia from your body. This usually happens when liver disease has reached its advanced stage. As such, ammonia levels may rise way above normal in your blood.
More so, people who have H.E also experience muscle wasting. This may also contribute to excess ammonia levels. How is this so? The muscle is one of the vital sites for ammonia removal outside the liver.
Since as far back as the 1930s, experts knew that ammonia is the main culprit in H.E. Since then, many doctors use serum ammonia as a way to diagnose and establish how severe H.E is. They also use it to monitor the treatment.
But the diagnosis of H.E is not only about ammonia levels. There are many other variables doctors must check. And there are also other dysfunctions they must first rule out.
There are three main places where your body breaks down ammonia. They are your liver, muscle, and brain. When the liver is no longer functioning as it should and there is muscle atrophy, the only organ left for ammonia breakdown is your brain.
In your brain, the astrocytes break down ammonia and make glutamine. But when too much ammonia is entering the brain, the astrocytes will also synthesize excessive amounts of glutamine. The excess glutamine, in turn, increases the inhibitory functions of GABA (gamma-Aminobutyric Acid).
As the astrocytes overwork themselves, trying to handle loads of ammonia coming into the brain, they would experience swelling. This comes with generating free radicals.
Excess GABA inhibitory function, free-radical generation, and astrocyte swelling combine and result in the cerebral dysfunctions that occur in H.E. These dysfunctions manifest as a wide spectrum of psychiatric or neurological abnormalities. The abnormalities can range from mild alterations to something as serious as a coma.
What Is Considered a High Level?
When ammonia levels (venous) are equal to or higher than 55µmol/L, there is a problem. It is at this point that doctors begin to check for possible signs of H.E, as well as other possible disorders.
However, there are a few things to consider when it comes to testing for ammonia levels. Multiple factors can affect how accurate the evaluation will be. For instance, if you clench your fist while they are drawing out your blood, it could falsely raise your ammonia levels. The same happens if the technician uses a tourniquet.
Aside from that, timing is also very important. Your ammonia levels depend on what time the laboratory processes your blood sample. They may get inaccurate if they do not immediately place your blood sample on ice. More so, they must centrifuge it within fifteen (15) minutes to get accurate results.
Now, even if they collect and process your blood sample properly, there are still concerns about how much correlation there is between H.E and ammonia levels.
A study checked out how sensitive and specific ammonia levels (venous) of 55µmol/L and above are for diagnosing H.E. The researchers found that that toxic level is only about 47 percent sensitive and about 78 percent specific.
The chance that a positive prediction from ammonia levels is indeed positive is 77.3 percent. But then, the chance that a negative prediction from ammonia levels is indeed negative is 48.6 percent. This gives ammonia levels a general diagnostic accuracy of about 59 percent.
This study showed that you can have H.E as severe as Grade 3 according to WHC grading and still have normal ammonia levels. You may also have high levels of ammonia, with no single sign of H.E. Meanwhile, there is no reason to suspect H.E except you already have chronic liver disease.
As such, you cannot bank on ammonia levels alone to diagnose H.E. Your doctor must check for other indices if you have high levels of venous ammonia, as well as rule out any other abnormality if you have any form of cerebral dysfunction.
Conclusion
Ammonia level in hepatic encephalopathy may be of value. But then, the result can sometimes be uncertain. However, physicians cannot ignore it because it remains a valuable index. When mental functions are altered, doctors will want to check if ammonia levels are normal. If there is a correlation, monitoring the changes in ammonia levels will help to know how well the treatment is working.