Pregnancy is an exciting time. With a little one on the way, many women are busy preparing for the new baby’s arrival. Though pregnancy is a natural process that the female human body is equipped for, it is not free of potential complications. Though rare, acute fatty liver of pregnancy is one of these possible complications.
Read on to find out what you need to know about acute fatty liver of pregnancy.
What Is Acute Fatty Liver of Pregnancy?
Before we go further, let’s discuss what acute fatty liver of pregnancy (AFLP) is.
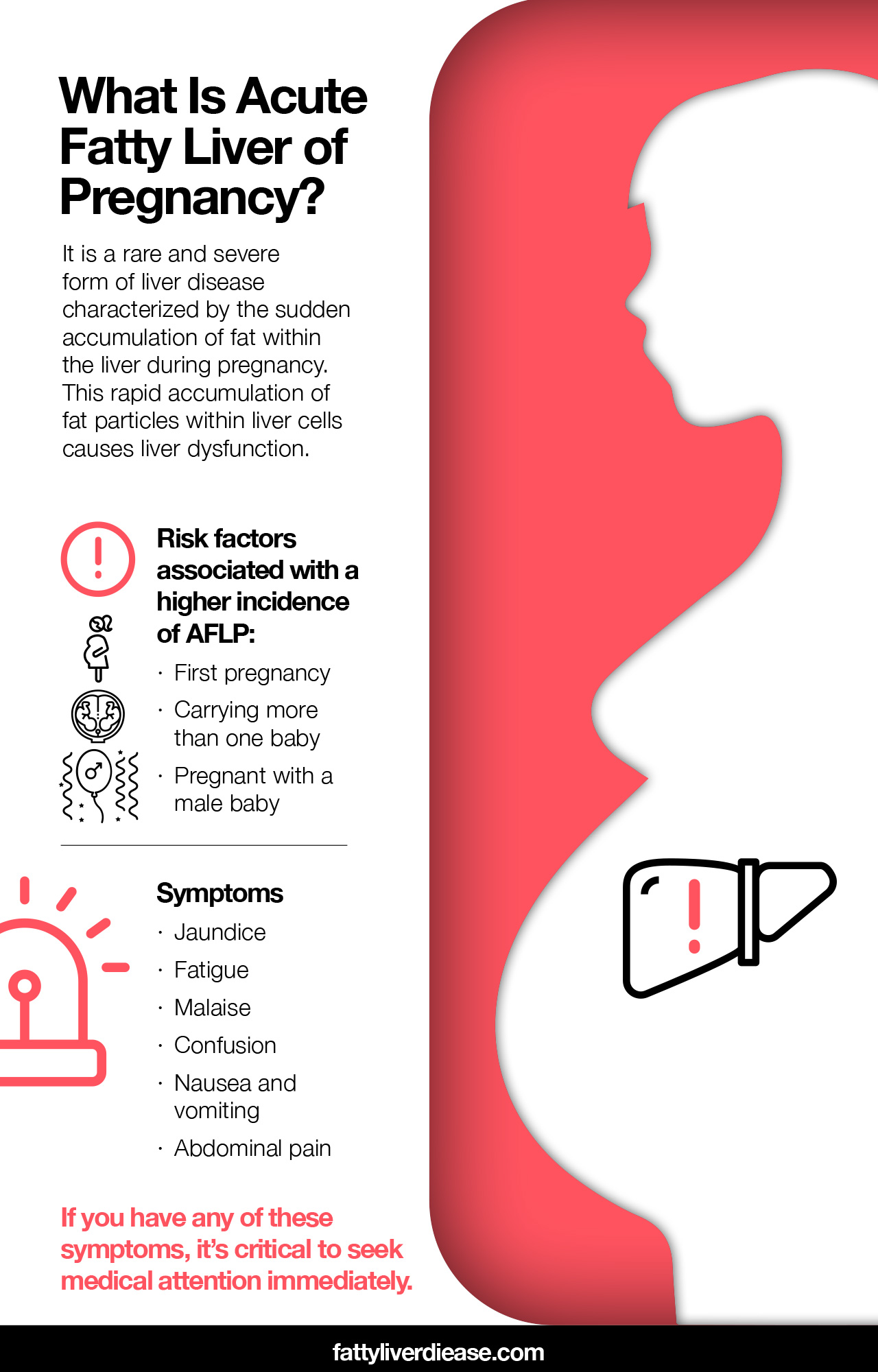
AFLP is a rare and severe form of liver disease characterized by the sudden accumulation of fat within the liver during pregnancy. The type of fat accumulation in AFLP is called microvesicular steatosis, which means that multiple tiny pockets of fat build-up within liver cells or hepatocytes. This rapid accumulation of fat particles within liver cells causes liver dysfunction.
AFLP usually develops during the third trimester of pregnancy, though it is possible to develop AFLP in earlier weeks of gestation. AFLP may be co-occurring with other conditions, including preeclampsia and hypertension, or high blood pressure. Hypoglycemia – or low blood glucose levels – is also typical in cases of AFLP. (1)
Because AFLP is a medical emergency, treating it often requires immediate delivery of the baby. Treatment may require a transfusion with blood and blood products. Though AFLP often resolves following delivery, in some cases, fat accumulation in the liver may continue in the postpartum time frame.
What Causes AFLP?
Doctors aren’t totally certain of the cause of AFLP in pregnancy, though it seems to evolve from metabolic dysfunction in both the mother and baby. In many cases, the pathogenesis of AFLP appears to be associated with a genetic deficiency of an enzyme called long-chain 3-hydroxyacyl CoA dehydrogenase (LCHAD). This enzyme is responsible for oxidizing fatty acids. When this enzyme is missing, fat particles are more likely to build up in liver tissue. When the growing baby cannot process certain fatty acids, they travel back to the mother via the placenta, potentially causing an accumulation of fat.
There also seem to risk factors associated with a higher incidence of AFLP: (1, 2)
- First pregnancy
- Carrying more than one baby
- Pregnant with a male baby
Symptoms of AFLP
If you have AFLP, you may notice a number of symptoms.
- Jaundice: When fat accumulates in the liver, the liver is no longer able to process bilirubin efficiently. The accumulation of bilirubin in the bloodstream causes the yellowing of the skin and whites of the eyes.
- Fatigue: Extreme tiredness is a common symptom of AFLP.
- Malaise: Feeling sick, having low energy, and having headaches are common symptoms that accompany AFLP.
- Confusion: When liver function is compromised, toxins may build up in the brain and cause mental symptoms like confusion.
- Nausea and vomiting: Loss of appetite, nausea, and vomiting are common with AFLP.
- Abdominal pain: Women with AFLP may experience liver pain, which can be felt in the upper right quadrant of the abdomen.
Complications of AFLP
Liver dysfunction, as a result of AFLP, can cause serious complications when not treated promptly. Compromised liver function may result in hepatic encephalopathy, which is the accumulation of toxic compounds like ammonia in the bloodstream. Ammonia interferes with normal mental functioning and causes anxiety, confusion, and seizures. Women with severe AFLP may also have pancreatitis, acidosis, intrahepatic cholestasis, and acute renal failure (or kidney failure).
AFLP may also present with a condition called HELLP syndrome, which encompasses hemolysis, elevated liver enzymes, and low platelets. AFLP also causes coagulopathy and disseminated intravascular coagulation, which are conditions that interfere with how the platelets in the blood clot. This results in excessive bleeding that can result in internal hemorrhage.
Diagnosis of AFLP
Doctors test for AFLP using a variety of diagnostic tools. Physicians will evaluate the clinical presentation, including symptoms of the disease.
Imaging like computed tomography (CT scans) and ultrasound can reveal the fatty infiltration of the liver and other abnormalities. Physicians may also administer a blood test to measure liver enzymes like aspartate transaminase (AST), alanine transaminase (ALT), and alkaline phosphatase (ALP). High liver enzymes in pregnancy suggest inflammation in liver tissue.
A liver biopsy is the most accurate way of diagnosing AFLP. A liver biopsy requires taking a tiny sample of liver tissue and evaluating it through a microscope. An analysis of the sample can reveal the presence of fat within liver cells.
Physicians specializing in obstetrics and gynecology, hepatology, and radiology will be involved in treating AFLP.
What to Do If You Think You May Have AFLP
If you are having symptoms of AFLP, it’s critical to seek medical attention immediately. Early diagnosis and treatment are vital for successfully managing AFLP. If you have AFLP, you are a high risk patient and will likely need to be admitted to the intensive care unit, because AFLP can be life-threatening for both you and your baby. Without prompt intervention, AFLP may result in hepatic failure or liver failure.
Acute Fatty Liver of Pregnancy: Conclusion
AFLP is a rare condition that occurs in pregnant women and causes the accumulation of fat within liver cells and subsequently compromises liver function. Though the incidence of AFLP is low across the general population, it’s still a good idea to be aware of symptoms and protocols for managing the condition. Once your case of AFLP has been treated and resolved, it’s important to receive proper supportive care to help minimize the risk of a possible future pregnancy.
References:
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2538964/
(2) https://www.stanfordchildrens.org/en/topic/default?id=acute-fatty-liver-of-pregnancy-90-P02465





















