Liver cirrhosis describes a disease condition where there is scar tissue in the liver. This scar tissue spreads across the liver and gradually takes the place of healthy, normal liver cells. The disease is progressive and may slowly develop over several years. If it is left untreated, the scar tissue will build up to a point that the liver will no longer be able to function. Before you can develop cirrhosis, there must have been continuous damage to your liver. It doesn’t just happen suddenly. The scar tissue will increase gradually with time. And by the time they begin to destroy and replace healthy cells, serious complications begin to show up. In this article, we will talk about cirrhosis diagnosis, as well as its causes and treatment.
Sometimes, scar tissue can block blood flow through and to the liver. This is a very fatal condition. It could also lead to eventual liver failure. Liver failure is a terminal condition. The thing, however, with cirrhosis is that symptoms do not show up on time. You may have it for many years and not even suspect that the disease is progressing on your body. So then, you must be able to recognize the risk factors for cirrhosis, as well as its subtle signs. This will help you detect the disease on time before it becomes an irreversible and terminal condition.
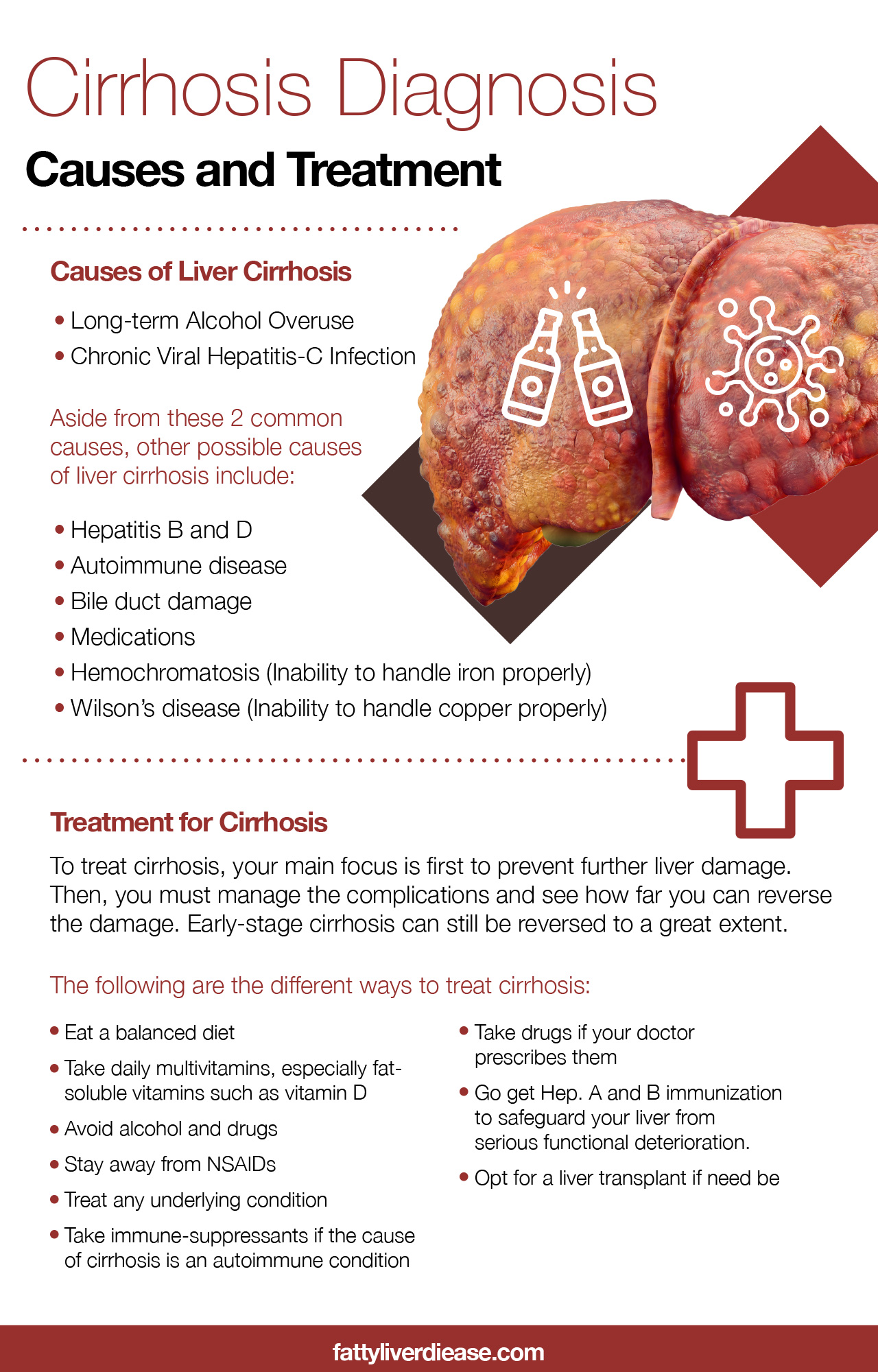
Causes of Liver Cirrhosis
What causes most cases of cirrhosis in the U.S are long-term alcohol overuse and chronic viral hepatitis-C infection. Obesity can also cause liver cirrhosis. However, this is not as frequent as alcoholism and hepatitis C.
If a woman drinks more than 2 cups of alcohol daily (including wine, beer, and liquor) for several years, she may develop cirrhosis. The same goes for a man who drinks more than 3 cups daily for several years.
It usually takes about 10 to 12 for people to develop cirrhosis from excessive use of alcohol. It is not a sure thing that those who drink too much alcohol for this long will have cirrhosis, but the risks are very high.
Hepatitis-C is a viral infection you can get from sexual intercourse. You can also get it if you expose yourself to infected blood. This can happen through needles that are contaminated, such as may come from piercing, tattooing, and IV drug abuse.
It is rare for someone to get Hepatitis C from a blood transfusion. The standards that blood banks use in the United States for screening donated blood are quite strict and rigorous.
Aside from these 2 common causes, other possible causes of liver cirrhosis include:
- Hepatitis B and D: Both of these forms of hepatitis cause inflammation in the liver, as well as liver damage. These can, in turn, cause cirrhosis.
- Autoimmune disease: Autoimmune conditions can cause inflammation in the liver (hepatitis). It is quite surprising that women make up 7 out of 10 people who have autoimmune hepatitis.
- Bile duct damage: Anything that damages the bile duct will end up affecting the liver. These ducts drain bile from your liver. So then, bile builds up in your liver, inflammation spreads, and cirrhosis may be the result.
- Medications: Medications, be it over-the-counter drugs or prescription drugs can cause liver damage if you use too much. Examples include common painkillers, antibiotics, some antidepressants, and so on.
- Hemochromatosis: Inability to handle iron properly
- Wilson’s disease: Inability to handle copper properly
Cirrhosis Diagnosis
The gold standard diagnostic test for cirrhosis is a liver biopsy. This is an invasive procedure, so it has some risks. A few serious complications can come from the procedure. That is why doctors only request biopsy if they are not sure what form of liver disease you have.
The doctor would ask for your medical history. He or she would also check your body for signs by physical examination. He may also request a few routine tests. These tests do not usually confirm cirrhosis, but they can help rule it out.
If at the end of the day, your doctor diagnoses cirrhosis, it doesn’t end there. Your doctor would order other lab tests to find out the extent (stage) of liver cirrhosis. These tests may also show if there are certain complications.
Furthermore, other tests may also help detect the cause of cirrhosis. Sometimes, there may be an underlying health issue that caused cirrhosis.
So the first thing your doctor would do is to take your personal and family history. If you have any of the risk factors, then your doctor may suspect cirrhosis. If some people in your family have had cirrhosis, then you may have some risk too.
During the physical examination, your doctor would watch out for a few signs. They include jaundice, ascites, and esophageal varices, among many others.
Another sign that may show up is called telangiectasias. These are markings that look like a small-sized red spider. These markings show up mainly on the chest. Telangiectasias are more common with those who have alcoholic cirrhosis, but those without cirrhosis or any other form of liver disease can have it too.
Other diagnostic tools that you doctor may use during his investigation may include the following:
- Magnetic resonance imaging scan (MRI scan)
- Computerized tomography scan (CT scan)
- Ultrasound
- Liver enzyme tests
- Blood albumin test
Treatment for Cirrhosis
To treat cirrhosis, your main focus is first to prevent further liver damage. Then, you must manage the complications and see how far you can reverse the damage. Early-stage cirrhosis can still be reversed to a great extent.
The following are the different ways to treat cirrhosis:
- Eat a balanced diet
- Take daily multivitamins, especially fat-soluble vitamins such as vitamin D
- Avoid alcohol and drugs
- Stay away from NSAIDs
- Treat any underlying condition
- Take immune-suppressants if the cause of cirrhosis is an autoimmune condition
- Take drugs if your doctor prescribes them
- Go get Hep. A and B immunization to safeguard your liver from serious functional deterioration.
- Opt for a liver transplant if need be
Cirrhosis diagnosis is more helpful if you find out in the very early stages. If you are finding out when it is already advanced, there is not much you can do. But if you find out early on, you may still be able to reverse the condition.