Lymphedema is a condition that affects the lymphatic system and usually results in swelling of an arm or a leg. Swelling can cause a significant amount of discomfort and affects your quality of life. Although there is no cure for lymphedema at this time, there are numerous ways to help manage the condition.
The lymphedema therapy regimen combines lifestyle, diet, physical therapy strategies, and sometimes surgery to help reduce swelling and increase mobility and comfort. Keep reading to find out what you need to know about lymphedema therapy entails.
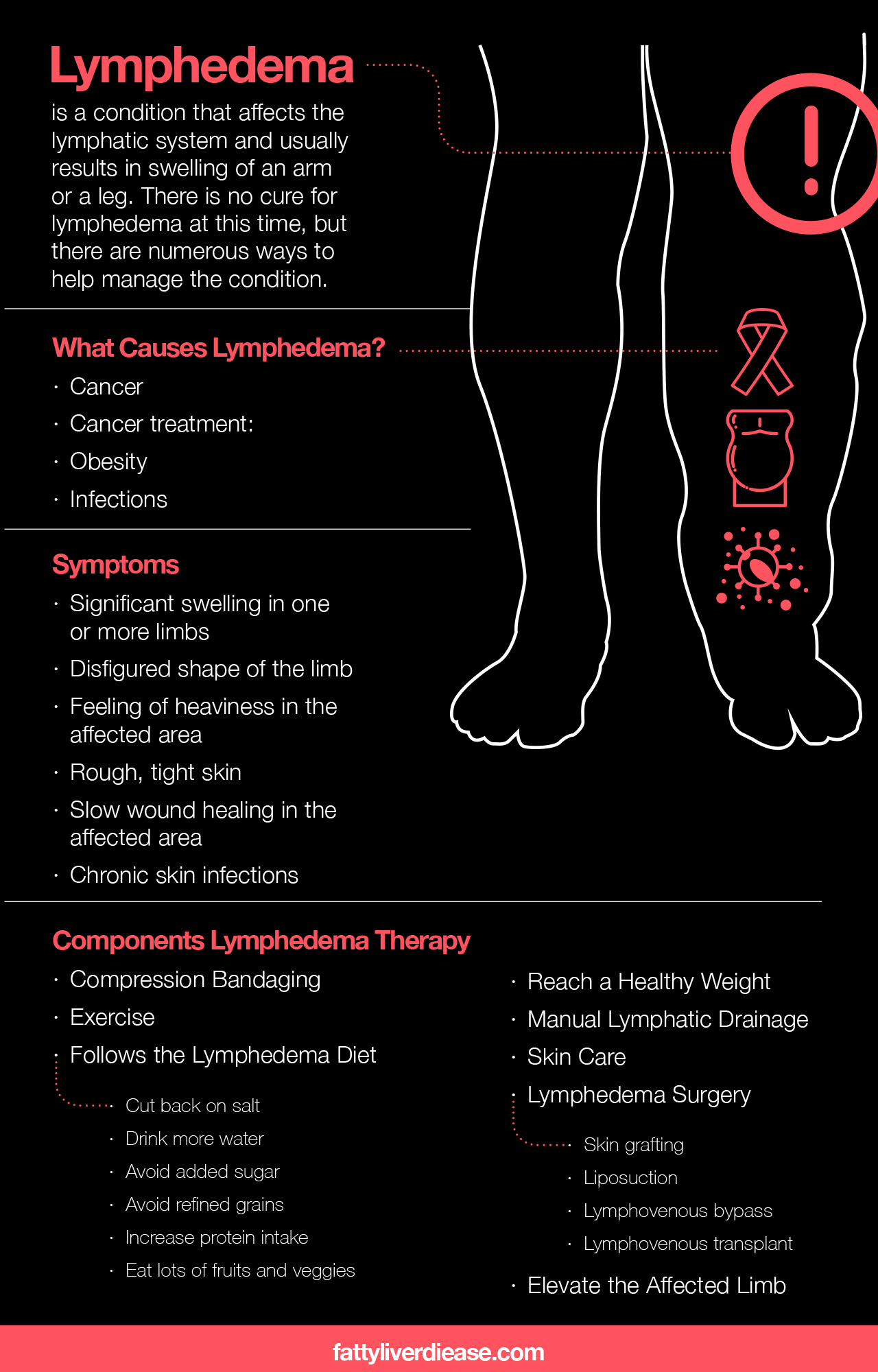
What Causes Lymphedema?
Lymphedema is a consequence of the inadequate circulation of the lymph system. The lymphatic system carries white blood cells and other cells of the immune system throughout the body to fight infection. The fluid then travels throughout the body and through the lymph nodes, which are responsible for filtering out waste from the lymph fluid. When the lymph vessels or the lymph nodes are damaged, lymph flow is inhibited, causing the buildup of excess fluid in the arms or legs. Although lymphedema most commonly affects the limbs, it can also affect other body parts.
Lymphedema is described as either primary lymphedema or secondary lymphedema depending on the root causes. Primary lymphedema occurs on its own without any other causal conditions. Secondary lymphedema is much more common and occurs as a result of other primary conditions.
Causes of lymphedema include:
- Cancer: Cancer cells travel through lymph fluid and can cause blockages in lymphatic vessels.
- Cancer treatment: Cancer surgery and treatments like radiation therapy remove lymph nodes and inflict damage on lymph nodes and lymph vessels. For example, breast cancer patients who have undergone a mastectomy tend to be at risk for lymphedema in the arms since the cancer removal surgery removes the lymph nodes present in the armpits.
- Obesity: Obesity is a significant risk factor that increases the risk of developing significant swelling as a result of lymphedema. Carrying excess fat cells is linked to the increase of inflammation in the body, as well as inflammatory conditions such as type 2 diabetes and fatty liver disease.
- Infections: Certain viral and bacterial infections can impede the normal flow of lymph fluid through the lymphatic system.
Symptoms of Lymphedema
In the early stages of lymphedema, you might not notice any symptoms at all. However, as lymph fluid continues to accumulate, you will begin to experience symptoms that can take a toll on your quality of life. Lymphedema symptoms may include:
- Significant swelling in one or more limbs
- Disfigured shape of the limb
- Feeling of heaviness in the affected area
- Rough, tight skin
- Slow wound healing in the affected area
- Chronic skin infections
Talking to Your Doctor
If you are experiencing symptoms of lymphedema or are concerned that you are at risk for developing it, it’s a good idea to make an appointment with your doctor. Your physician will review your medical history and your symptoms. If you receive a lymphedema diagnosis, you will be given a lymphedema treatment plan.
Keep in mind that if you have recently been diagnosed with cancer or you have undergone cancer treatment, you will likely be given guidance for prevention strategies as well as lymphedema treatment.
Components of Lymphedema Therapy
Knowing what to expect during lymphedema treatment can be very helpful as you plan your treatment.
1. Compression Bandaging
Compression bandaging is a helpful strategy for reducing swelling in the affected limb. Compression garments and bandaging are effective for increasing blood flow and preventing blood clots when sitting or standing for prolonged periods of time. They are also effective for improving the flow of lymph fluid and preventing significant swelling in the affected arm or leg. A health care provider will give you direction for how to wrap compression bandages so that they are effective.
2. Exercise
One of the most effective ways of increasing the circulation of lymph flow in the body is by exercising. Increasing physical activity helps blood and lymph fluid circulate more fully. If you have lymphedema, it’s important to be cautious when first starting to exercise, especially if you are recovering from other conditions such as cancer or heart disease. Do not immediately dive into a vigorous workout routine.
Instead, start out with slow, calm movements. Most exercises designed for lymphedema won’t be very strenuous. Instead, they will be gentle and aimed towards getting the fluid in your body circulating more effectively. Even adding stretching techniques or other very gentle exercises into your daily routine can make a big difference for lymphedema.
If you are movement-restricted, a physical therapist can give you exercises that work for your limitations while also improving lymphedema. It’s best to check with a physical therapist, doctor, and lymphedema specialist to ensure that you are doing exercises that work best for your specific needs. Always make sure that your lymphedema exercises are cleared by your doctor so that you’re not putting too much stress on your system.
3. Following the Lymphedema Diet
The foods you eat can affect lymphedema. Following dietary guidelines can help you reduce swelling and manage lymphedema more effectively. Here are a few of the guidelines that your health care provider may give you to help manage lymphedema.
- Cut back on salt. Eating too much sodium can cause your body to retain excess water. When the body holds onto water, this can negatively impact blood pressure and worsen swelling associated with lymphedema.
- Drink more water. Staying hydrated helps all of your body’s cellular processes function smoothly while also increasing circulation and flow of lymph fluid and blood.
- Avoid added sugar. Eating too much added sugar can cause a variety of health problems such as fatty liver disease, insulin resistance, and type 2 diabetes. Eating too much sugar can also increase the levels of systemic inflammation in the body, which can damage the lymph system and worse and lymphedema.
- Avoid refined grains. Limiting the consumption of confined grains in your diet can help you manage your lymphedema. Refined grains are converted into sugar by the body and directly contribute to inflammation. Limit your intake of white rice and white bread and instead eat whole grain products like quinoa and brown rice.
- Increase protein intake. The essential amino acids in protein help your body repair the damage to soft tissue that lymphedema causes. Eating high-quality protein is also important for supporting the immune system and healing from injury and disease. Furthermore, eating lots of protein helps you feel more full which can facilitate weight loss.
- Eat lots of fruits and veggies. Fruits and vegetables are packed with micronutrients such as vitamins, minerals, and antioxidants and help reduce systemic inflammation in the body. Reducing systemic inflammation and oxidative stress can help repair damaged lymph vessels while also improving the flow of lymphatic fluid.
4. Reaching a Healthy Weight
If you are significantly overweight or obese, losing weight can help manage lymphedema by relieving pressure on the lymphatic system and reducing inflammation. Monitoring calorie intake, eating primarily whole foods, and increasing your activity levels are effective and sustainable strategies for reaching and maintaining a healthy weight. A registered dietitian or nutritionist can help you follow the best weight loss strategies for your specific needs.
5. Manual Lymphatic Drainage
Manual lymphatic drainage (MLD) is a form of complete decongestive therapy (CDT) that treats lymphedema. MLD is administered by a certified lymphedema therapist, who has a full understanding of how to manipulate the flow of lymph fluid throughout the body.
MLD is essentially a form of massage that helps manually move lymph fluid from the limbs and other affected areas back towards the heart so that it can circulate more effectively. In some ways, MLD is much like a massage. Sessions with your certified lymphedema therapist will likely begin and end with deep breathing techniques, which can help relax the body and improve the flow of lymph fluid and your body‘s response to MLT.
Your lymphedema therapist will also teach you drainage techniques that you can administer at home on your own.
6. Skin Care
Skin care is a vital part of the lymphedema treatment plan. When lymphedema progresses, it can cause significant tightness, scarring, scaliness, and redness on the skin of the affected area. Growths may also develop on the surface of the affected limb.
When taking care of the skin on your swollen limb, it’s particularly important to prevent infection. Areas of the body affected by lymphedema are particularly prone to chronic infections since there is inadequate circulation of immune system cells. You can help reduce the risk of infection by protecting the area from cuts and scratches and keeping the skin clean and dry.
Keeping skin moisturized can help prevent cracking and bleeding. Regularly apply a moisturizer to help prevent the skin from breaking.
7. Lymphedema Surgery
In severe cases of lymphedema, surgical treatment of lymphedema may be the best option. There are different types of surgery that your physician may recommend to manage your lymphedema.
- Skin grafting: Skin grafting is a surgical mechanism of repair that replaces damaged tissue with healthy tissues.
- Liposuction: Severe lymphedema, in addition to fluid build up, may also cause the accumulation of fat cells in the affected area. Liposuction can help reduce the size of the limb affected by lymphedema.
- Lymphovenous bypass: In a lymphovenous bypass procedure, the surgeon essentially re-routes lymph fluid around damaged areas. This allows lymph fluid to flow uninhibited.
- Lymphovenous transplant: Also known as a vascularized lymph node transfer, a lymphovenous transplant involves replacing damaged lymph nodes with healthy ones from another area of the body.
8. Elevating the Affected Limb
Your physician may recommend elevation as a way of encouraging lymph fluid circulation. Gravity can play a big role in worsening lymphedema by pulling fluids downwards into the lower part of the limbs. When standing and sitting, blood and fluids are more likely to pool towards the feet and hands. If the lymph system is not working properly, lymph vessels are unable to effectively remove the excess fluid. You can counteract some of this pooling by elevating your feet and arms whenever you are sitting or lying down. It’s especially beneficial to raise your legs and hands above the heart when lying down.
Things to Keep in Mind
No two cases of lymphedema are the same. Different underlying causes and different areas of the body may be affected, depending on the individual. As a result, it’s important to always follow your doctor’s advice when managing your lymphedema.
Lymphedema Therapy Takeaways
Lymphedema is a complex condition that usually accompanies other primary conditions, like cancer, infection, and inflammation related to obesity. Though there is no lymphedema cure, you can manage the condition by incorporating diet, lifestyle, and exercise strategies into your daily routine. Compression bandages, manual drainage, and exercise help increase the flow of lymph fluid while eating lots of protein and cutting out sodium help to manage swelling. By consistently incorporating these therapeutic strategies into your daily routine, you can fight lymphedema and significantly increase your quality of life.