Our heart rate is in a healthy range when it is neither too fast nor too slow. Tachycardia is the term for a heart rate that is too fast, while bradycardia describes the opposite condition. What does it mean to have a low pulse rate, and is it something you should be worried about? Keep reading to find out the answers to your questions.
What Exactly Is Bradycardia?
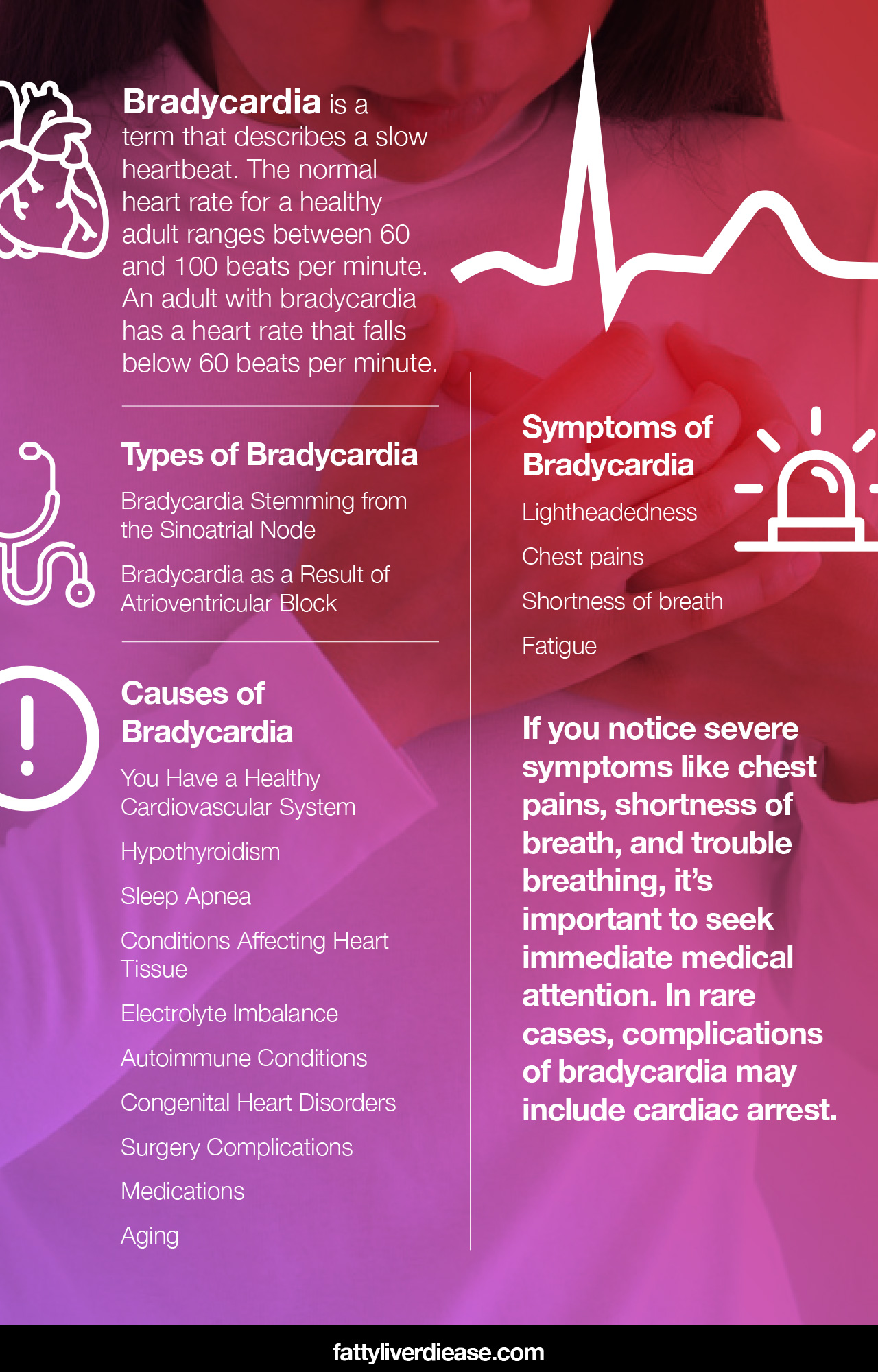
Bradycardia is a term that describes a slow heartbeat. The normal heart rate for a healthy adult ranges between 60 and 100 beats per minute. An adult with bradycardia has a heart rate that falls below 60 beats per minute.
Before we dive into the different types of bradycardia, let’s take a look at the electrical activity of the heart. The heart is sectioned into four chambers. The two lower chambers are called the ventricles, while the two upper chambers are the atria. Electrical signals that stem from the right atrium are responsible for regulating heart rate. The specific area of the right atrium responsible for producing these signals is called the sinoatrial node (also referred to as the sinus node or SA node).
Electrical signals from the SA node then travel to the atrioventricular node (AV node), which then sends the electrical impulses to the ventricles. The ventricles direct blood that has been depleted of oxygen to the lungs and direct oxygenated blood throughout the body.
Interferences in this electrical system result in issues with heart rate, including bradycardia.
Types of Bradycardia
There are two main types of bradycardia, depending on the root cause of the slow heart rate.
Bradycardia Stemming from the Sinoatrial Node
This type of bradycardia, often called sinus bradycardia, is caused by an abnormality in the sinoatrial node. The SA node is often referred to as the heart’s natural pacemaker and is responsible for regulating the heart’s electrical system and heart rate.
The sinoatrial node may cause bradycardia by initiating consecutive electrical signals at a slower rate. The sinoatrial node may also initiate signals more unpredictably or erratically. Or, signals coming out of the sinoatrial node may be blocked. As a result, these blocked signals don’t trigger a heartbeat.
Bradycardia as a Result of Atrioventricular Block
When bradycardia results as a result of an atrioventricular block, electrical signals may be leaving the sinoatrial node normally. However, these signals essentially get lost in translation before they reach the ventricles. There are varying degrees of heart block, depending on the severity and whether there are accompanying symptoms.
First-degree heart block generally causes no symptoms. In the case of first-degree heart block, all electrical signals from the sinoatrial node make their way to the atrioventricular node, though impulses may be occurring at a slower rate. If no symptoms are present, and you are young and physically active, first-degree heart block may not require any treatment at all.
In the case of second-degree heart block, not all electrical impulses from the sinoatrial node make their way to the atrioventricular node. These “blocked” signals can result in a long time in between heartbeats, causing a slower heart rate. Sometimes, second-degree heart block can cause arrhythmia, which is an irregular heart rhythm.
Third-degree heart block is the most severe form of heart block. In the case of third-degree heart block, none of the sinoatrial node’s electrical signals make it to the ventricles. A natural, autopilot pacemaker system kicks in when electrical impulses don’t get to the ventricles. However, the heart may beat or slowly and sometimes irregularly.
Symptoms of Bradycardia
In many cases, bradycardia will not cause any symptoms and is not a cause for concern. However, in other cases, bradycardia causes insufficient amounts of oxygen-rich blood to reach certain parts of the body. When tissues and organs do not receive enough oxygen, symptoms arise.
Bradycardia may be accompanied by:
- Lightheadedness
- Chest pains
- Shortness of breath
- Fatigue
If you notice severe symptoms like chest pains, shortness of breath, and trouble breathing, it’s important to seek immediate medical attention. In rare cases, complications of bradycardia may include cardiac arrest.
Causes of Bradycardia
What causes bradycardia? There are several potential causes of bradycardia, and in many people, bradycardia is actually a good thing!
You Have a Healthy Cardiovascular System
Keep in mind that bradycardia may simply be the product of a healthy cardiovascular system instead of a diagnosable issue. If that is the case, the heart is so efficient that when at rest, it does not require more than 60 beats per minute to sufficiently distribute oxygen and nutrient-rich blood to all parts of the body. Healthy bradycardia is most common among physically active young adults and athletes. Bradycardia in these circumstances is also desirable because a slower resting heart rate helps reduce the amount of wear and tear on your heart muscle over time.
Hypothyroidism
Hypothyroidism describes low thyroid function. Hypothyroidism is a condition that affects the thyroid gland and upsets your body’s hormone balance. If you have hypothyroidism, your body doesn’t produce sufficient levels of triiodothyronine and thyroxine, both of which are important for regulating your heart rate. In addition to bradycardia, individuals with hypothyroidism often experience fatigue, weight gain, and persistent feelings of being cold.
Sleep Apnea
Bradycardia is commonly caused by sleep apnea. Sleep apnea occurs when you momentarily stop breathing during sleep, causing oxygen levels to dip below a normal, healthy level. When oxygen levels dip, the body responds by lowering the heart rate to conserve energy. Sleep apnea is associated with obesity and metabolic conditions and can cause complications when untreated for a prolonged period of time.
Conditions Affecting Heart Tissue
Infections or other damage to heart tissue can interfere with the heart’s ability to regulate the pulse rate. Heart attacks, coronary artery disease, and infections of the heart tissue like myocarditis can all interfere with the electrical impulses that cause your heart to beat.
Electrolyte Imbalance
The flow and concentration of minerals in the bloodstream and within cells play a critical role in regulating electrical signaling that causes the heart to beat at a regular rhythm and at an appropriate rate. Sodium and potassium are particularly important minerals in this process. Any type of fluid loss – such as sweating, vomiting, and diarrhea – can all cause electrolyte imbalances.
Electrolyte imbalances can be rectified by drinking plenty of water supplemented with electrolyte tablets. Eating foods rich in potassium and consuming a balanced amount of sodium can help ensure that you’re getting the minerals that you need.
Autoimmune Conditions
Certain autoimmune conditions such as lupus may impact your heart rate. An autoimmune condition develops as a result of environmental and genetic factors that influence your immune system’s function. An autoimmune disease occurs when the immune system begins attacking the body’s healthy tissue instead of only launching attacks against foreign invaders and harmful cells like it’s supposed to. Autoimmune diseases may affect any area of the body, such as the heart. For example, lupus may cause inflammation of heart tissue, which can cause bradycardia.
Congenital Heart Disorders
A congenital heart disorder is a heart defect that is present at birth. Such heart conditions may affect structural or electrical components of the heart and have the potential to cause issues like bradycardia or arrhythmias.
Surgery Complications
Heart surgeries may result in heart rate abnormalities. If you’ve recently undergone heart surgery and have bradycardia, consult your surgeon and physician.
Medications
Certain medications may affect heart rate. Bradycardia is a potential side effect of medications that treat arrhythmias, psychotic disorders, and hypertension. If you’re on any of these medications, consult your physician. If a slow heart rate is a side effect of a medication you are taking, your physician will be able to prescribe a medication that effectively treats your condition without causing bradycardia. For example, beta-blockers and calcium channel blockers are commonly prescribed to treat high blood pressure and can be associated with bradycardia. Your physician may prescribe a different kind of beta-blocker or an alternative medication to treat your condition.
Aging
Bradycardia may also simply result from the aging process. As we age, cells and tissues begin to function less efficiently over time. This is why our hair turns grey, and our skin begins to wrinkle. Aging affects not only our outward appearance but also the function of organ systems like the cardiovascular system. Aging may cause damage to heart tissue as a result of wear and tear over a number of years.
Make an Appointment with Your Physician
If you are noticing a slower heart rate than usual and related symptoms, it’s a good idea to visit your doctor. He or she will conduct a physical exam and listen to your heart using a stethoscope and assess any symptoms that you may be having. Based on an assessment and your medical history, your physician may refer you to a cardiologist.
What to Expect at the Cardiologist
A cardiologist is a medical specialist in the field of cardiology and assesses and treats conditions affecting the heart and circulatory system. When you visit a cardiologist’s office, information must first be gathered about your heart function. This can be done through an electrocardiogram (EKG or ECG) and an echocardiogram (commonly called an echo).
An EKG can be done in the doctor’s office and gathers electrical information from your heart for about 12 seconds. However, if you don’t have chronic bradycardia, 12 seconds may not be ample time for the EKG to pick up on it. In this case, the cardiologist may want you to wear a Holter monitor for 24 hours or longer. A Holter monitor is basically an EKG that gathers electrical information about your heart over a longer period of time, which increases the likelihood that any abnormal heart rhythms will be detected. Wearing a Holter monitor is preferred for patients who experience intermittent symptoms.
An echocardiogram uses ultrasound technology to examine structural aspects of your heart, such as valve shape and blood flow. An echocardiogram can help determine if there is any inflammation or damage to blood tissue. Your cardiologist will also need blood tests, your medical history, and a medication list to make sure there are no other underlying conditions or risk factors affecting your heart health.
Does bradycardia always need to be treated? Not necessarily. If you are a young and athletic person, bradycardia is healthy. Additionally, if your case of bradycardia is not causing any symptoms, you might not require treatment. Your physician and cardiologist will be able to assess your health and determine whether your case of bradycardia is normal and healthy or if it requires treatment.
Looking After Your General Heart Health
Regardless of what is causing bradycardia, protecting your heart health is important. Healthy lifestyle and diet choices play an important role in making sure your heart is strong.
- Exercise: Does exercise help bradycardia? Though exercise may not directly help bradycardia, it definitely helps strengthen your heart and promote a healthy blood pressure and circulatory system. The more you exercise, the stronger your heart muscle gets. As you get increasingly physically fit, your resting heart rate will go down. This is because your heart muscle will be able to more effectively circulate blood and oxygen throughout the body with each pump.
- Cutting down on saturated fat: Cutting out saturated fat in your diet is vital for protecting heart health. Saturated fat is known to increase cholesterol levels in the bloodstream. When your cholesterol levels are too high, this can cause cholesterol and other particles in the blood to congeal and form plaques on the walls of arteries and blood vessels. The formation of these plaques is called atherosclerosis. Over time, the accumulation of plaques in the bloodstream can increase your risk of heart attack, stroke, and heart disease. You can decrease your intake of saturated fat by cutting out fatty animal products in your diet. For example, this means illuminating red meat, sausages, bacon, ham, processed meats like salami, whole milk, butter, and cheese.
- Reducing alcohol intake: We usually consider Alcohol as a substance that primarily impacts the liver. However, the consumption of lots of alcohol can also impact the heart. Drinking excessive amounts of alcohol can actually cause damage to the heart muscle as well as the electrical signals that cause our hearts to beat regularly. Aim to limit your alcohol consumption to one drink per day at the most.
- Cutting down on sodium intake: Sodium is a major part of the western diet. You can find sodium in a number of staple foods, such as meat, cheese, and other processed foods. Sodium causes problems in the cardiovascular system because the consumption of excess sodium drives blood pressure. When we are carrying excess sodium in our bloodstream, the body tends to hold onto extra water to help maintain the homeostasis of the blood. However, higher blood volume means that more pressure is exerted against arterial walls, which raises blood pressure. Over time, high blood pressure can contribute to inflammation of the blood vessels, which can impact the heart and weaken the heart muscle over time. To reduce your dietary sodium intake, aim to avoid processed foods like chips, cured meats, restaurant foods, and fast foods.
- Eating plenty of protein: We normally think of proteins as benefiting our muscles in our bodies, such as our biceps or quadriceps. But did you know that the heart is also a muscle and requires dietary protein? Dietary protein is so important because it supplies essential amino acids, which are vital for replacing old muscle tissue, maintaining muscle mass, synthesizing new connective tissue, supporting immune function, and producing neurotransmitters and enzymes. Even more importantly, we must get optimal ratios of essential amino acids on a daily basis in order to most effectively support all of these biological processes. Optimal ratios of essential amino acids are available in single animal sources of protein, such as meat and dairy. However, because it’s crucial to avoid saturated fat to protect your heart health, stick to lean meats like chicken breast, egg whites, and fatty fish. You can also get optimal ratios of essential amino acids from eating a primarily plant-based diet. The only catch is that when getting your protein from plant-based foods, it’s important to eat a variety of vegetable proteins throughout your day, such as whole grains, beans, nuts, and seeds.
Precautions
What heart rate is an emergency when you have bradycardia? It can be very difficult to put cut off numbers on heart rates. This is particularly true because each person has their own normal range, depending on genetics, age, and activity levels. Plus, if at any point you are concerned about your heart, it’s a good idea to make an appointment with your physician. Getting your heart checked out can help determine if there’s something to be worried about, or it can simply be reassuring.
Conclusion: What Causes Bradycardia?
In many cases, bradycardia is absolutely nothing to worry about and instead is a sign that your heart is functioning very efficiently. In other cases, bradycardia may be the result of sleep apnea, heart conditions, thyroid function, electrolyte imbalances, and congenital abnormalities. Only a doctor can determine whether your specific case of bradycardia requires diagnosis and treatment. So if you are experiencing bradycardia accompanied by concerning symptoms, be sure to seek medical attention. Regardless of the underlying cause of bradycardia, it’s always a good idea to follow a heart-healthy diet rich in fruits, vegetables, and essential amino acids.